
And how constipation, prostate inflammation, and “rockiness” problems are all directly related…
—-Important Message—-
This is the fun DIY activity that got me huge results in bed

All my problems with going soft and struggling to stay “rocky” and feeling numb down there…
Completely gone thanks to this fun little do-it-yourself activity.
Before this, I tried hypnosis, I tried pills, I tried pumps…
I wish I had known that this simple at-home activity was all I needed.
———-
What is really causing your constipation
It’s common knowledge that hypothyroidism can lead to weight gain and obesity…
Yet few people realize it’s also a cause of constipation.
This is a very consistent link.
And since hypothyroid people aren’t necessarily overweight, then constipation could be the most obvious feature.
In other words, constipation could be notifying you of a bigger problem.
A canary in the coal mine, so to speak.
However, triiodothyronine (T3) production is dependent on the intake of certain dietary “minerals”…
So hypothyroidism is fortunately an easy fix for most people.
Excluding the presence of antithyroid antibodies (as in Hashimoto’s disease), often, hypothyroidism is made even worse from an iodide and/or selenium deficiency.
We need iodide, of course, to make thyroxine (T4), a hormone produced by the thyroid.
And we need selenium for the enzyme that converts it into triiodothyronine (T3).
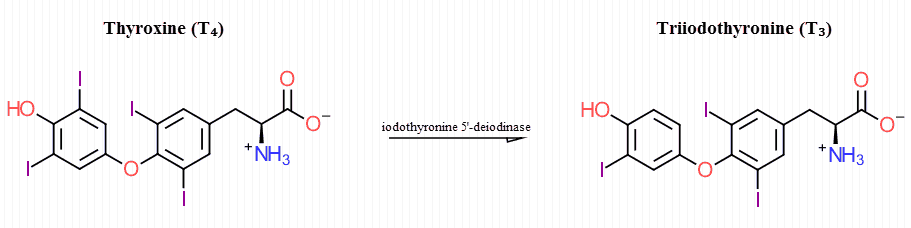
Triiodothyronine (T3) is the fully active form of thyroid hormone and has one less iodine atom than thyroxine (T4).
This transformation is executed by the selenoenzyme iodothyronine 5’‑deiodinase.
This enzyme is the reason why selenium deficiency can also cause hypothyroidism.
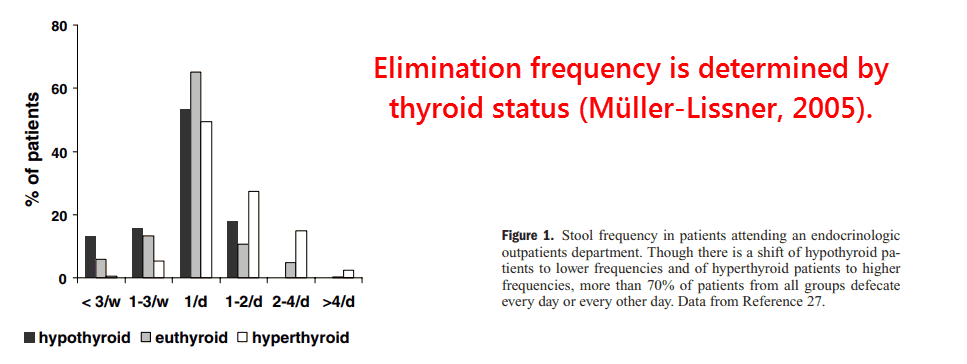
And as you’ll see, hypothyroidism very consistently leads to constipation.
That much is nearly certain…
Though the means by which this occurs has never been formally proven.
Regardless, there’s reason to believe that hypothyroid‑induced constipation occurs via increased alpha-2 adrenoceptors in the intestines, brain, and enteric nerves.
The alpha-2 adrenoceptor is an inhibitory receptor capable of inducing constipation, similar to the μ‑opioid receptor (a.k.a. MOR) in effect.
Thyroid hormones are known to modify the distributions and types of adrenoceptors throughout the body.
And that is just one mechanism out of many through which they control metabolism.
So, besides intestinal methane and diet‑derived exorphins, or opiate peptides, hypothyroidism is another reliable cause of constipation.
Here is some evidence to that effect:
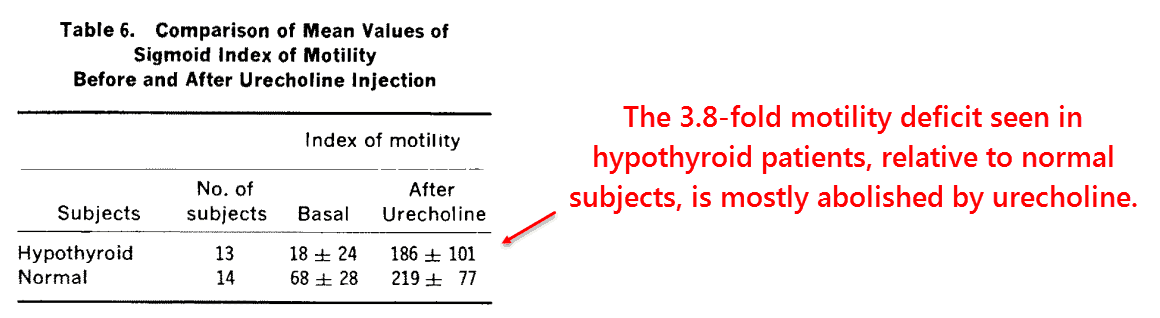
On account of the historical case reports linking hypothyroidism to constipation, these scientists decided in 1971 to conduct the first modern study.
They recruited 73 patients with hypothyroidism to study motility. (Motility has to do with metabolic energy.)
To do this, they used pressure transducers and radio telemetry capsules.
They also performed post‑mortem examinations on 30 others subjects.
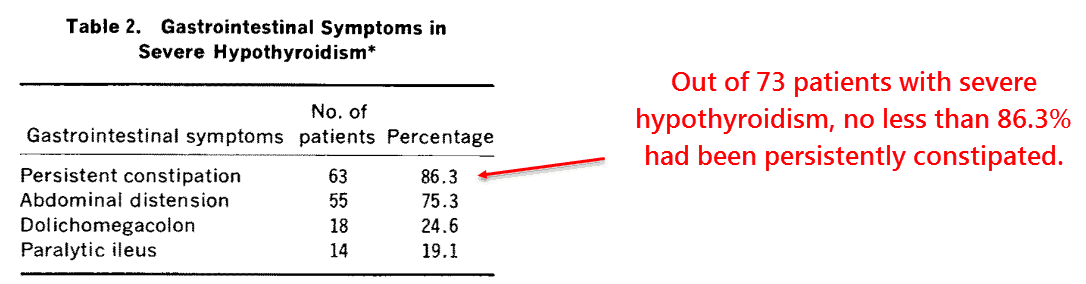
They found a significant reduction of motility in the hypothyroid subjects, both in the colon and the small intestine.
And they described some minor histological changes upon autopsy.
Although thyroid hormone increases the aquaporin‑8 water channel, which could be thought to account for the constipation…
But the fact that nerves are involved precludes that mechanism.
“The mean jejunal rhythm was 7.5 cycles/min in hypothyroid patients compared with 12 cycles/min in normal subjects.”
Studies on hypothyroid dogs (1977) confirm the electrical nature of the problem, as do studies with hypothyroid rats (1992).
Further implicating the nervous system is the observation that urecholine virtually obviated this motility deficit.
Urecholine specifically activates muscarinic acetylcholine receptors responsible for motility.
The finding that hypothyroid subjects achieved nearly the same motility as controls with the drug implies the problem lies on the neurotransmitter level.
And thyroid hormone is known to affect only one of all neurotransmitter systems in the body.
Triiodothyronine (T3) consistently regulates receptors of the adrenergic system, including the inhibitory alpha-2 adrenoceptors central to motility.
The fact that urecholine could reverse this deficit is entirely consistent with this:
It has been shown that alpha-2 adrenoceptors cause constipation by inhibiting the release of acetylcholine.
And it makes sense that this would be offset by cholinergic drugs such as this.
“However, the fact that the colon…was capable of a normal response suggests that the smooth muscle was fundamentally intact but that there was some disorganization of normal control mechanisms.”
The regulation of alpha- and beta-adrenoceptors by thyroid hormone is well established and predictable.
However, the levels of alpha-2 adrenoceptors have never been examined in the hypothyroid intestine.
This is because more attention is directed at examining alpha-1 and beta-1 adrenoceptor numbers in the liver, adipose tissue, erythrocytes, and brain.
The intestine is one organ that is relatively ignored in this regard.
The same is true of alpha-2 adrenoceptors in general.
Yet circumstantial evidence indicates that hypothyroidism does cause elevated levels of these:
Upon clonidine administration, hypothyroid subjects have been observed to have twice the response than hyperthyroids.
This was true among all parameters tested:
- Concentrations of noradrenaline (delta Na)
- Mean arterial pressure (delta MAP)
- Pulse rate (delta pulse rate)
All of these parameters changed more in the hypothyroid state.
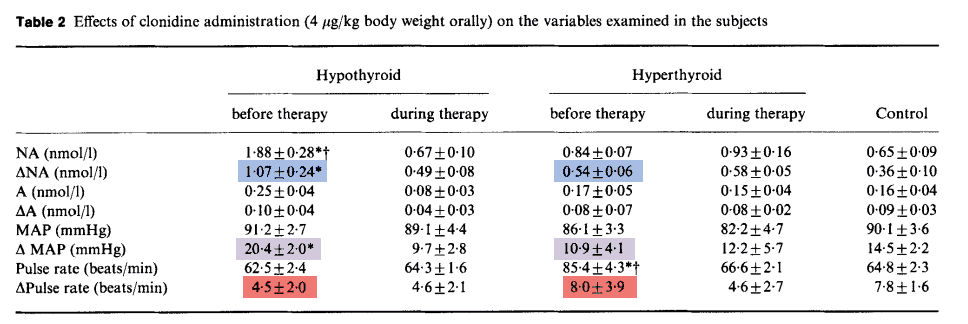
The release of catecholamines from the adrenal medulla is controlled by alpha-2 adrenoceptors.
And clonidine is a specific alpha-2 agonist.
From this, you could infer that hypothyroidism is accompanied by increased alpha-2 adrenoceptor expression…
If true, this could account for the reduction of motility characteristic of the condition.
This is because alpha-2 adrenoceptors are also present in the intestine and have a negative influence on colonic motility:
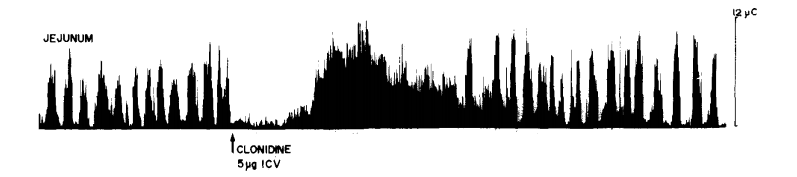
This is one study out of dozens demonstrating that alpha-2 adrenoceptors exert powerful control over intestinal function.
They used alpha-2 agonists such as clonidine, alpha-2 antagonists such as yohimbine, and rats with surgically implanted electrodes.
They found that injections of clonidine, a drug that crosses the blood-brain barrier, would essentially paralyze the small intestine.
This is what you’d expect from a stress hormone.
Adrenaline has been shown to constrict certain blood vessels, through alpha-1 and beta-1 receptors, while relaxing other ones through beta-2 receptors.
The net effect of adrenaline is to increase blood flow to the muscles and brain…
…at the expense of organs of less immediate importance – such as the skin and kidneys.
Digestion doesn’t seem to have high priority in times of stress…
That’s also the case with things such as hair growth, collagen synthesis, and glomerular filtration (glomerular filtration has to do with production of urine).
They found that the alpha-2 antagonist yohimbine could largely offset the effect of clonidine on intestinal function…
This effect depended on where it was injected – yohimbine does not cross the blood-brain barrier.
Intramuscular injection of yohimbine was able to prevent the reduction of intestinal tone induced by clonidine…
But it couldn’t stop it from disrupting the contractile rhythm.
Conversely, yohimbine injections into the brain did the opposite…
It would prevent the rhythmic disruption, yet couldn’t prevent the direct reduction in tone.
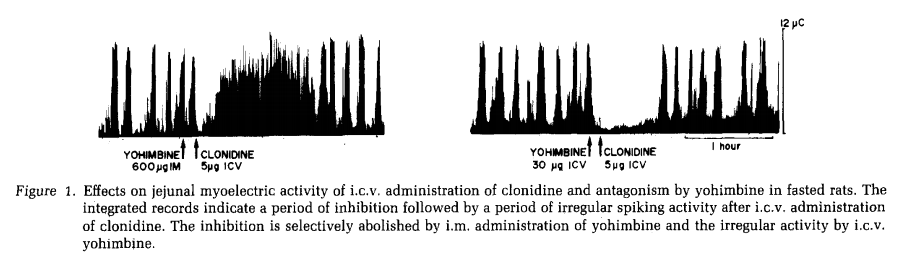
This study shows that alpha-2 receptors work to inhibit motility in both the intestines and the brain…specifically in the regions that innervate the digestive tract.
It also shows that the rhythmic contractile response is under the control of adrenaline and noradrenaline.
Medical professionals use clonidine to lower blood pressure.
In those situations, it has been reported to cause severe constipation.
Clonidine also reliably “treats diarrhea”…
And studies indicate it does this by reducing motility – not through increasing absorption.
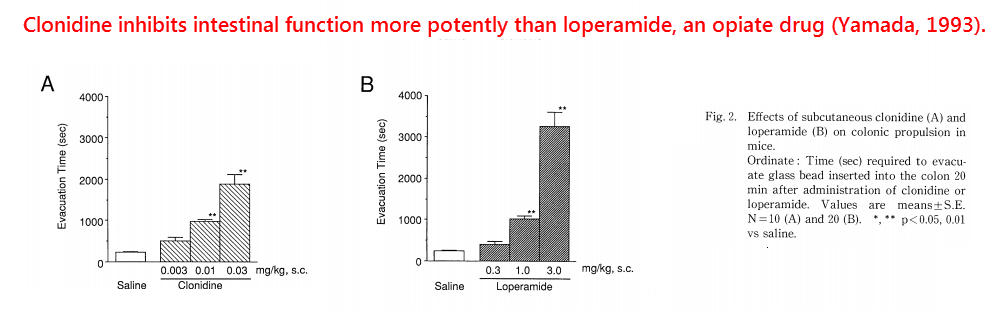
On the other hand, yohimbine has been shown to reverse constipation in some people.
Yet, since it also blocks alpha-2 receptors on the adrenal medulla, it can increase adrenaline and actually cause constipation.
So taking the iodide + selenium combination should be more reliable, and may also eliminate other symptoms of hypothyroidism.
So alpha-2 regulation of intestinal motility is well‑established.
And it is just as physiologically important as μ‑opiate receptors (MOR) in its effect.
The low G.I. function seen in hypothyroidism is just as well‑established.
Of course, correlation doesn’t prove causation.
But this study below does prove causation…
This study involved 15 hypothyroid patients made “normal” through thyroxine replacement.
They initially measured small intestinal motility using the hydrogen breath test.
And they did this again upon restricting thyroxine for only one week.
The result was a near‑doubling of intestinal transit.
This effect reverted back to normal a week after the treatment stopped:
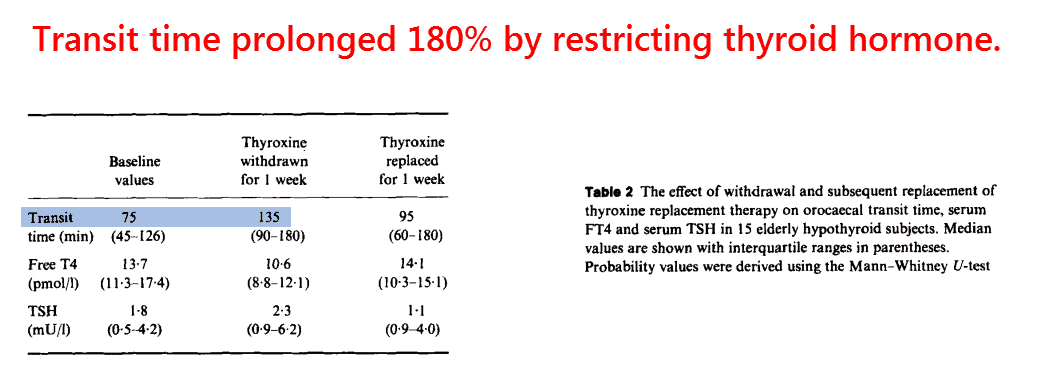
This is more proof that hypothyroidism is a direct cause of constipation, and another indication of its neurotransmitter basis.
The fact that this happens so quickly all but rules out other proposed mechanisms (e.g. hyaluronic acid accumulation).
Countless studies show that thyroid status regulates beta-adrenoceptors – so many that there are review articles on the topic.
And there is every reason to suppose it does this by upregulating alpha-2 adrenoceptors in the intestines…especially considering the hypothyroid response to clonidine.
Hypothyroidism is often caused by iodide deficiency, selenium deficiency, or some combination of both.
This can be an easy fix. And these are two dietary “minerals” that everyone should be taking anyway. But don’t take too much of either one — they can become toxic.
I prefer getting iodine and selenium from natural foods rather than supplements. Eating wild seafood (squid, octopus and my personal favorite oysters) is the best way to get enough of these nutrients.
—-Important Message about Thyroid—-
Have you heard about this lifespan breakthrough — CID5920 — that lets men live decades longer with a happy, healthy, and sexy life?

Until now, CID5920 was kept secret and only given to rich celebrities and powerful politicians…
But now men like you and me can start taking it right away and reap the rewards…
I don’t know about you, but I’ve been waiting for this day for a long time…
Because once you discover all of the incredible benefits of CID5920, you will wish you had it 20 years ago…
Don’t worry though — if you start it now you could still live 20 or 30 years longer and with amazing sexual prowess of a young man…
Remember: no one knows how long CID5920 will be available… they could snatch it away again at any time…
Here’s how to get CID5920 now before it’s gone again.
———-
