
…the best way for men to keep a young mind and memory…

—-Important Message—-
My testosterone went from 600 to 883 with this one vitamin
Ron was taking T supplements for 5 years. Now his T has skyrocketed — and he stopped the injections and supplements.
Here’s his secret…
It’s all about this newly discovered vitamin.
Most doctors don’t know about this vitamin yet.
This strange vitamin makes the Leydig cells activate — those are the testicle cells that produce testosterone and other male androgens.
Here’s what Ron had to say about raising his T naturally:
Here’s the strange vitamin and it’s crazy discovery story that skyrocketed Ron’s testosterone.
———-
This simple vitamin raises brain adrenaline and prevents dementia
It’s now fairly well established that dementia patients are often characterized by 1 of the following:
- reduced acetylcholine receptors in the forebrain
- low B vitamins
- high homocysteine
- previous and/or current aluminum exposure
Yet an overlooked characteristic of dementia is reduced brain adrenaline, a neurotransmitter intimately associated with planning and learning.
This is an important finding because the more dementia is understood, the more measures can be confidently applied to prevent it.
And as with acetylcholine, the biochemical pathways behind low brain adrenaline have been progressively worked-out over the past 50 years.
Adrenaline biosynthesis relies on certain food-factors that many people, and especially older ones, tend to be deficient in.
‘Senile dementia of Alzheimer’s type (SDAT) is consistently associated with damage to the cholinergic projection to cerebral cortex and hippocampus, […] In addition there have been several reports of a loss of pigmented neurones from the noradrenergic nucleus, locus coeruleus, in brainstem in SDAT [13, 6, 8, 13],’ ―Iversen
So besides using nootropic drugs like vinpocetine and galantamine to maintain memory and intelligence, nutritional supplements or dietary changes can also be helpful.
But first comes the evidence:
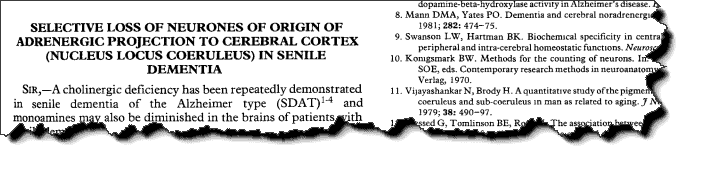
This brief report summarizes a study that had compared postmortem cell counts of 20 patients diagnosed with Alzheimer’s against 10 controls.
The locus coeruleus was examined. This is the center of brain adrenaline distribution.
This brain structure sends out projections to other regions, regulates attention, and has been shown to divert blood flow and glucose to the most active areas.
The locus coeruleus prioritizes brain energy, and uses adrenaline and noradrenaline to accomplish this.
Electrode studies on non-human primates show this area is highly involved in correct decision making.
Studies on humans consistently reveal an important function in memory retrieval.
This study here found a bit of variance in the demented and control subjects, with cell counts of the locus coeruleus ranging from 1,013 to 12,890.
And because the data implied a division, they broke the dementia subjects into 2 groups:
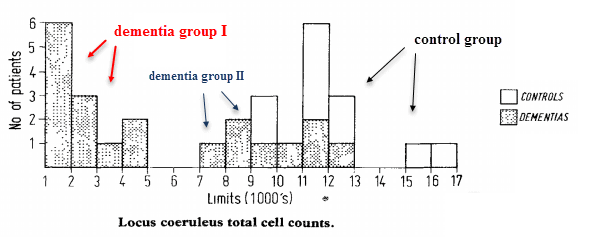
One group is borderline normal, overlapping the control group.
Yet the other group is far more extreme and characterized by profound reductions of cell count.
The group involving the more drastic reductions—group I—was also characterized by more severe dementia. And moreover, this group had also died younger, so this effect was independent of age.
‘The differences in cell count between groups I and II are therefore the reverse of those which would have been expected if they had been due to ageing.’ ―Bondareff
These results would imply that reduced brain adrenaline is not exactly caused by aging, but IS a notable characteristic of high-grade dementia.
Now this is what you’d expect after reading experimental studies on the locus coeruleus, the brain structure perhaps just as involved in memory retrieval and executive function as the cholinergic system.
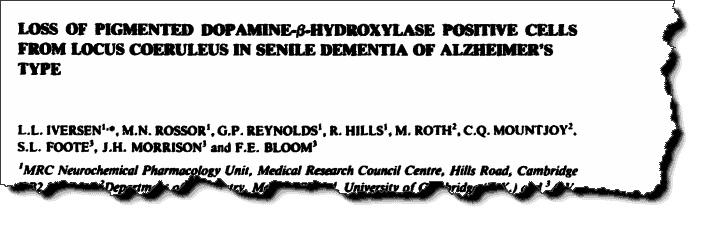
Other studies show similar findings, like this one which had also measured neurotransmitter concentrations:
Postmortem brains had been obtained, sectioned, and stained with antibodies that bind specifically to dopamine-β-hydroxylase.
This is the enzyme that converts dopamine into noradrenaline, so it makes sense that they would use it to mark adrenergic brain cells.
The locus coeruleus is highly enriched with this enzyme, which is found scant in few other regions of the brain.
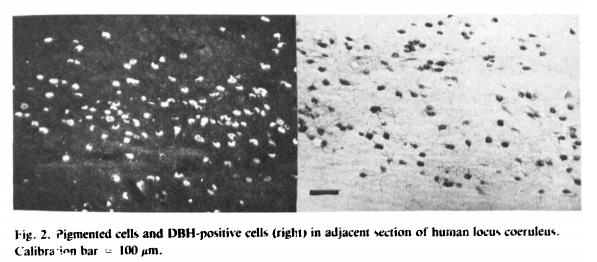
The scientists found similar cell counts as the other study, ranging from 1,185 to 12,078, and they also discovered these numbers correlated with dementia severity.
The control cases had cell numbers ranging from 7,884 to 12,078 while the Alzheimer’s patients had them between 1,185 to 5,390 (excluding one outlier).
The average cell counts between the two groups was 9,426 vs 4,075.
‘The extent of this loss varied considerably among the SDAT group, with an average reduction in locus coeruleus cell population of about 60%,’ ―Iversen
They had also measured concentrations of noradrenaline and dopamine.
Since these neurotransmitters are the product and substrate of dopamine-β-hydroxylase, respectively, you might expect to find decrements in the former.
This was in fact the case. Noradrenaline had been found radically lowered in Alzheimer’s patients versus the controls, yet with no reduction at all in dopamine — which is more of a Parkinson’s trait.
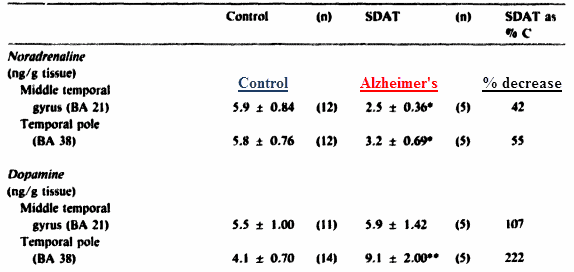
This is consistent with reduced dopamine-β-hydroxylase activity.
Coincidentally, reduced dopamine-β-hydroxylase activity was also found lowered in dementia using enzyme kinetic studies.
‘The loss of noradrenaline was selective as cortical dopamine concentrations were not decreased, or were even unexpectedly increased in patients with SDAT.’ ―Iversen
Now if a person were to hypothesize a reason for a molecular imbalance of this type, the most straightforward mechanism would be a reduction in the enzyme’s cofactor—should it have one.
And it does: dopamine-β-hydroxylase has a cofactor called vitamin C.
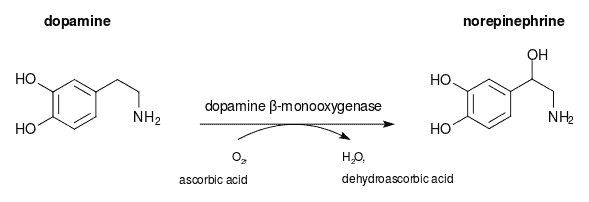
It is somewhat well-known that adrenal glands have an unusually high concentration of vitamin C, yet a fact often overlooked is that the brain also needs it to synthesize adrenaline.
Experiments on guinea pigs, which cannot synthesize vitamin C, and rats, reveal that subclinical scurvy has profound implications for brain adrenaline synthesis.
So just as in the adrenal glands, vitamin C is a significant determinant of adrenaline concentration in the brain.
They made guinea pigs marginally deficient by restricting vitamin C for 2 weeks. After this initial period, the guinea pigs were subdivided into 4 groups.
Group 1 received the stock Purina® guinea pig pellets that were measured to contain 0.5mg per gram of vitamin C.
The other 3 groups received pellets similar in composition but lacking in vitamin C.
To prevent clinical scurvy: group 2 was supplemented a full 10mg per day, group 3 was given 10mg per kilogram body weight, and group 4 received 5 mg per kilogram body weight.
After 10 to 12 weeks on this regimen, the rodents were sacrificed via decapitation, and brain dopamine and noradrenaline were then determined by the method of Jacbowitz and Richardson.
After an initial decline in brain noradrenaline (norepinephrine) during the depletion period, the neurotransmitter had returned to baseline in the 2 groups consuming the most vitamin C:
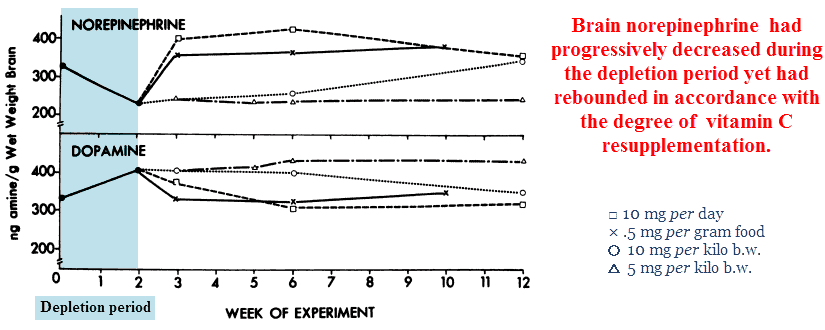
The guinea pigs consuming the least vitamin C — group 4 — remained stuck at levels nearly half that of the vitamin-replete group.
And just like the Alzheimer’s cases above, dopamine increased as a result of a reduced conversion to noradrenaline.
‘Figure 8 illustrates that brain norepinephrine and dopamine levels change in response to brain ascorbate depletion, and on repletion of ascorbate catecholamine values return to within normal ranges.’ ―Hoehn
Now these guinea pigs didn’t exhibit any visible signs of scurvy, they were merely suffering from a low-grade form.
Group four had consumed 5mg per kilogram body weight every day, equating to 400mg for an average-sized human (175 pounds).
This is still 6 to 7 times the recommended daily average in the United States, a value set criminally low.
Millions of Americans and Europeans are consuming ascorbate at this low level right now, and just like guinea pigs they cannot synthesize vitamin C either.
Based both on primitive diets and the synthesis rates of other animals, it has been calculated that the average human ought to consume between 2.3 and 4.0 grams per day.
But you don’t necessarily have to stop there. Higher amounts have been safely taken and are sometimes even suggested during infection.
Vitamin C is also needed for collagen synthesis, and can even increase brain noradrenaline in animals which synthesize their own.
This was a very simple study primarily involving rats, a spectrophotometer, and a massive 500 mg⁄kg injection of vitamin C.
Rats make their own vitamin C, so they should have plenty…yet despite this fact, their brain adrenaline & noradrenaline increased.
The author noted increased vitamin C concentrations in the brain, increased noradrenaline, and also the reduction in dopamine you’d expect from increased β-hydroxylase activity.
‘From Table 1 it can be seen that ascorbic acid decreased dopamine and at the same time increased noradrenaline in some cerebral structures, as early as 5 min after injection.’ ―Izquierdo
Perhaps also worth mentioning is that adrenal catecholamines hadn’t changed a bit. This implies that peripheral synthesis was already operating at the maximum rate.
It could appear that the adrenals get more than their fair share and the brain whatever remains.
Although this could be the best all-around strategy for survival, it does imply that brain synthesis isn’t operating at maximum capacity even during natural vitamin C intakes.
The fact the adrenals retain so much vitamin C could be why this effect has been largely overlooked. If peripheral adrenaline synthesis only decreases with ascorbate levels low enough to cause scurvy, then low brain adrenaline might falsely be assumed to operate in the same way.
‘Ascorbic acid produces an increase in the concentration of ascorbic acid in the brain; this rise was not observed in the adrenal medulla where the concentrations of catecholamines were also unchanged.’ ―Izquierdo
If guinea pigs are any indication of what happens to humans, brain catecholamine levels will fluctuate under normal dietary intakes.
This means that in addition to the classic dementia-associated vitamins — e.g. thiamine (B1), folate (B9), and cobalamin (B12) — a deficiency in vitamin C may also have implications for this condition.
And to convert noradrenaline into adrenaline we do need 2 others, namely folate (B9) and cobalamin (B12).
These 2 vitamins are the cofactors for methionine synthase, the enzyme responsible for regenerating methyl groups and reducing homocysteine.
After S-adenosylmethionine is re-methylated by methionine synthase and vitamins B9 and B12, it can then be used as a cofactor in phenylethanolamine N-methyltransferase (PNMT).
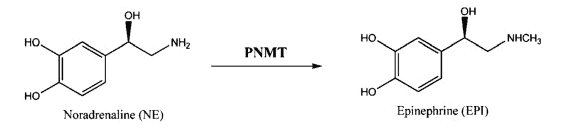
This step is also important because adrenaline (epinephrine) works primarily on α‑adrenergic receptors, the type most involved in memory retrieval.
Norepinephrine certainly is active, for sure, yet this catecholamine has more affinity for the β-adrenergic receptors.
Folate (B9) and cobalamin (B12) are commonly found reduced in dementia and are also used to explain the condition.
Because ethanolamine requires a sequential addition of 3 methyl groups to become choline, any disruption in the brain methyl pool reliably lowers acetylcholine (and also melatonin).
‘Both folate and cobalamin deficiencies may cause similar neurological and psychiatric disturbances, including depression, cognitive deterioration, and demyelinating myelopathy.’ ―Nilsson
Thiamine (B1) is involved mainly because it provides the acetyl group for acetylcholine, yet it does also increase general glucose consumption.
Beriberi, Wernicke encephalopathy, and Korsakoff syndrome are forms of thiamine deficiency named before the common cause had been discovered. All 3 conditions are characterized by cognitive impairment.
Thiamine and vitamin C are the 2 most heat-labile vitamins, so besides refined foods not contributing much, any cooked food will have diminished amounts.
So I think it’s fair to conclude that either a proper whole-food diet or supplementation are required for ideal brain function.
While ‘nootropics’ operate on adrenergic & cholinergic systems and certainly do help with cognition and memory, it’s always good to have these vitamins for backup, or at least for their other functions.
‘Depletion of ascorbic acid resulted in decreased concentrations (25%) of norepinephrine in the brain.’ ―Hoehn
—-Important Message for Men Who Want to Prevent Cognitive Decline—-
My SUPER C is 100x more potent and powerful than regular vitamin C — increases brain adrenaline and protects mind and memory

You may have heard that the problem with regular vitamin C is that it doesn’t stay in the body long enough for you to benefit…
And it’s true. Your body eliminates it in under 5 minutes (as you can see when you pee).
Which is why I’ve developed a different type of vitamin C that stays in the bloodstream for HOURS not minutes.
And that way it has time to benefit all the organs, especially the brain.
I call it Super C and it can:
- Reduce inflammation by 45%
- Increase brain adrenaline, may prevent dementia and Alzheimer’s
- Improve blood flow all over the body
- Naturally lower blood pressure
- Boost the body’s natural immunities
- …and so much more…
Try my powerful Super C today for free
———-
