
It calms the cytokine storm and stops the sickness in its tracks
—-Important Message From Our Sponsor—-
Your heart uses 13 pounds of this one molecule — are you deficient?

If you don’t know how to support the production of this molecule…
You’re leaving yourself and your loved ones open to BIG problems.
You see, my own father suffered a heart attack…
The doctor said he would never fully recover…
But as a health researcher, I refused to take this news sitting down.
In fact, my research shows there’s one simple way to cut the recovery time after a heart attack by 88%.
I showed my father… and youthful energy sprung out of him like the Bellagio Fountains in Vegas.
Now he’s playing with his grandkids for hours like he used to.
I found him chopping wood again, just barely breaking a sweat.
Even his skin seems to glow with health!
So today, I’m trying to share my story with anyone who will listen.
I’m revealing the full name of this special molecule AND how to support it — 100% free.
———-
Study: This one simple vitamin is a perfect antiviral treatment
When it comes to preventing respiratory viral infections, few things can compete with vitamin D3.
This is because plasma vitamin D3 levels have been consistently correlated with the risk of viral infection, as have polymorphisms of the vitamin D receptor.
Vitamin D3 is also what best explains the well‑known seasonal fluctuations in influenza rates.
Although low humidity also plays a role by keeping viruses airborne longer, it’s difficult to deny that vitamin D3 contributes more heavily — there is simply so much evidence.
Moreover, what’s known about the effects of vitamin D3 on human physiology is entirely consistent with this.
It’s been known for over a century that sunlight cures both tuberculosis and rickets, two conditions with widely disparate etiologies.
Little did researchers know back then that just one vitamin can fully explain BOTH effects.
The calcemic effects of vitamin D3 were discovered as far back as the ’30s, thus providing an explanation for rickets…
Yet it wasn’t until 2004 that its specific effects on the immune system had been elaborated.
This study was inspired by the previous finding that the gene encoding cathelicidin, an antimicrobial peptide, contains a vitamin D response element.
This would suggest that this peptide is controlled through the vitamin D receptor, yet of course that needs to be tested to know for sure.
So they had added 1,25‑(OH)‑vitamin D3 to cells and confirmed that they would, in fact, produce cathelicidin in response. This had occurred even at the low concentration of 1nM, and in all six cell lines tested:
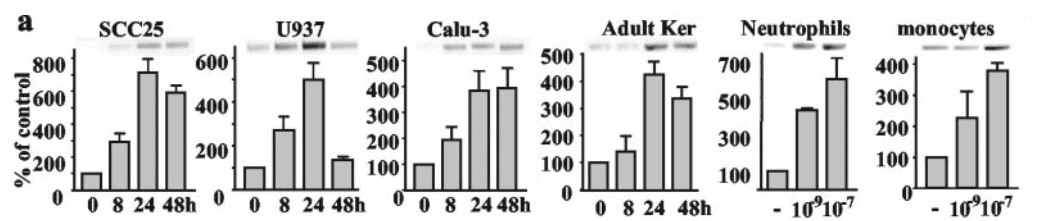
So this antibacterial effect occurs everywhere active vitamin D3 is found.
These cell lines derived from the lung, skin, and tongue as well as the immune cells types: monocytes, neutrophils, and macrophages.
These are exactly the types of the cells you’d want producing antimicrobial peptides to defend against viruses, especially respiratory ones.
Since lung epithelial cells have been shown to convert vitamin D3 into its fully active form, you could rightly expect this to occur in vivo from supplementation or sunshine.
This is supported by the fact that cathelicidin has been detected in nasal and bronchial secretions associated with mucin.
Cathelicidin has well‑established antibacterial activity so it provides a perfect explanation for the effect of sunlight on tuberculosis.
But what about VIRAL respiratory infections?
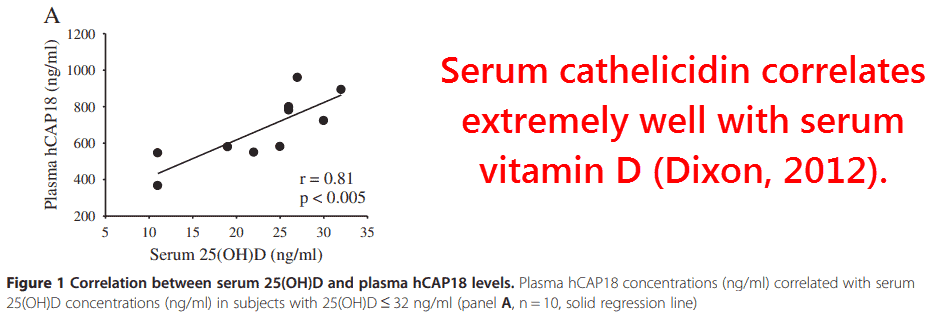
Cathelicidin can also explain the effects of vitamin D3 in this regard because it’s been consistently shown to be antiviral.
This idea that vitamin D3 is effective in vivo has been demonstrated by the use of the active form, calcitriol.
In one study, administering calcitriol had increased the percentage of subjects with detectable cathelicidin in their airways from 7% to 90%.
Not surprisingly, this increased cathelicidin had correlated with reduced incidence of respiratory infections.
So there’s every reason to believe that the antiviral peptide cathelicidin can ultimately explain the periodicity of influenza rates because it lies downstream of vitamin D3 which, in turn, is affected by seasonal changes in sunlight.
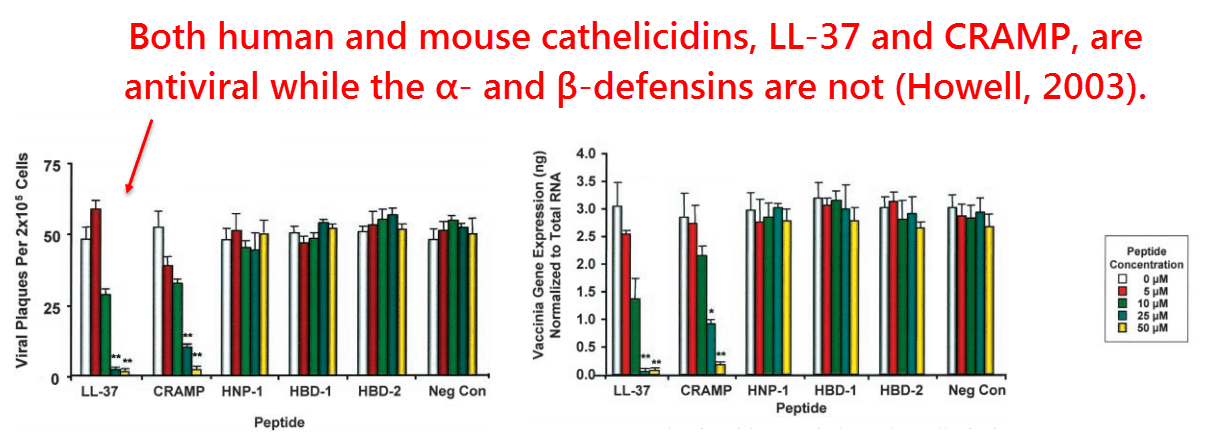
So this cathelicidin in the airways provides the first‑line defense against inhaled viruses, along with enzymes myeloperoxidase and lysozyme.
The fact that it’s ultimately cathelicidin doing this has recently been proven without a doubt using mice, influenza virus, and inhaled peptides:
All mice had been divided in four groups and then given nebulized H1N1 influenza virus:
- One was a control group
- One was a cathelicidin group
- One a zanamivir group
- And one a scrambled peptide group
All treatments were aspirated in the mice’s lungs one day before the virus was administered, and then once again seven days afterwards.
The groups of mice showing increased survival were the treatment groups, as expected, but somewhat surprising was that cathelcidin had performed as well as the antiviral treatment zanamivir.
Or perhaps it’s better stated the other way around, with it being surprising that zanamivir had performed as well as cathelicidin…
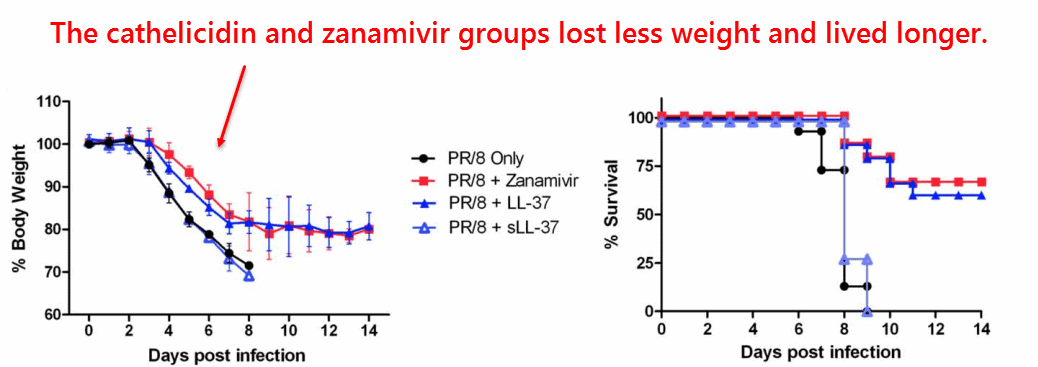
Lung viral titers had also decreased in the cathelicidin (LL‑37) and zanamivir groups while the scrambled peptide (sLL‑37) again offering no protection.
There were also changes in cytokines, most notably reductions in IL‑1β.
“[…] the therapeutic use of LL‑37 was able to reduce the severity of the influenza virus infection to a similar extent as the well characterized antiviral ‘treatment’ zanamivir, a current first‑line therapeutic.” ―Barlow, 2011
This reduction in IL‑1β is quite important and parallels the other beneficial function of vitamin D3, namely, the ability to tame overactive immune responses during respiratory infection.
It is known that the fatalities caused by most if not all respiratory viral infections can be attributed to cytokine storm, not the virus itself.
So virus infections are similar to fatal septic shock in the way they can become fatal.
Although fatal septic shock is most often caused by BACTERIA invading the body, it can be caused by purified LPS — a nonliving substance.
This demonstrates that it’s the immune system that kills people, not bacteria, per se.
So the perfect antiviral treatment would prevent cytokine storm and also inhibit the virus.
There is actually a considerable amount of evidence that vitamin D3 can do just that, making it the single best substance to take for viral prevention.
This study was a natural continuation of earlier work showing that vitamin D3 is converted into its active form in lung cells.
They’d then confirmed some of their prior results of vitamin D3 but on another cell line this time, human tracheobronchial epithelial cells.
They had also discovered a few more effects, most notably that 25‑(OH)‑vitamin D3 inhibits NF‑κB signalling by upregulating its binding protein IκBα.
This is important because NF‑κB is ultimately responsible for transcribing some of the most pathogenic enzymes including: 5‑lipoxygenase, iNOS and cyclooxygenase‑2.
Furthermore, the inhibition of NF‑κB caused by vitamin D3 hadn’t interfered with viral clearance.
The amount of viral RNA had remained largely unaffected by vitamin D3 relative to the control, yet its infectivity actually did decrease some — perhaps by upregulating cathelicidin.
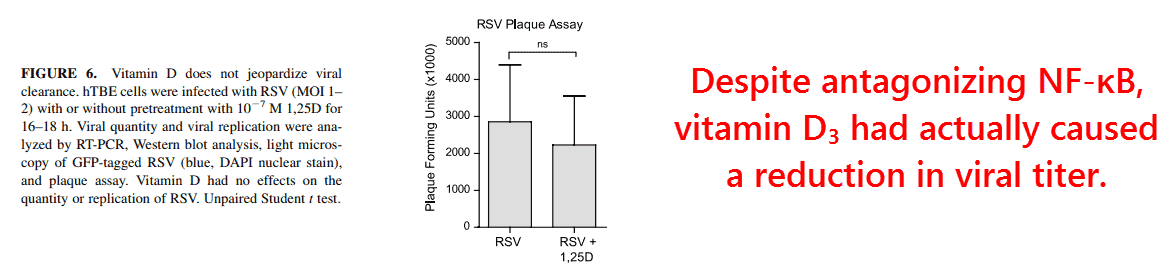
It was also shown that 1,25‑(OH)‑vitamin D3 had no negative effect on the signalling of type‑I interferons, the most specific cytokines for viral defense.
Interferons were in fact discovered for their ability to inhibit viral replication, and for good reason. Nearly every enzyme induced by interferons acts to either destroy or inhibit the replication of viral RNA.
“Vitamin D did not suppress IRF-3 translocation to the nucleus but, on the contrary, may have even increased it.”
Interleukin‑1β on the other hand is not specific to viruses, but to bacteria.
This can be inferred by just considering two enzymes it upregulates, 5‑lipoxygenase and hepcidin.
The former is responsible for synthesizing leukotriene B4, a chemoattractant molecule for eosinophils & neutrophils into the airways.
Naturally, these bacteria & fungi‑specific immune cells would do more harm than good against viruses as they replicate INSIDE of cells.
Interleukin‑1β also upregulates hepcidin, a regulatory hormone that reduces iron absorption.
This is ostensibly done to inhibit bacterial growth by limiting an important mineral, yet this would have no effect on viruses since they could care less about iron.
Interleukin‑1β also upregulates ferritin, a protein which further restricts free iron.
Due to the lower production of hemoglobin you expect from this, IL‑1β could further compromise oxygen delivery in patients with pneumonia.
It could be worth noting that vitamin D3 has been shown to decrease hepcidin and increase hemoglobin in mechanically ventilated adults.
Researchers did not measure cytokines in that study, yet it would seem consistent with its ability to lower IL‑1β.
Another clue about the teleological role of interleukin‑1β is the manner in which it’s induced.
It’s been shown that its induction is primarily accomplished through toll‑like receptor‑4, the main LPS sensor in our body, and mediated through NF‑κB.
Lipopolysaccharide is of course specific to Gram‑negative bacteria, not viruses, another observation that implies that any interleukin‑1β created during a viral infection is inappropriate at best.
More indication is given by the finding of elevated levels of the cytokines IL‑1β, TNF, IL‑6, and IL‑4 being the best predictors of death during acute respiratory distress syndrome.
“A plasma IL‑1β or IL‑6 level >400 pg⁄mL on any day in the first week of ARDS was associated with a low likelihood of survival.” ―Meduri, 1995
The fact that cytokine storm itself can cause death calls into question the inherent pathogenicity of respiratory viruses.
That is to say, most of these viruses could be harmless were it not for them being able to activate TLR‑2 — i.e. somewhat like “tricking” the body into thinking they’re bacteria.
This idea that the immune response is more harmful than the virus is supported by the fact that SARS is always cultured using vero E6 cells, the only cell line where it shows cytopathic effects.
This is of course done to make infection easy to detect, yet it also implies that infection from this virus could be completely insignificant in the absence of an immune system.
If the virus itself doesn’t damage lung cells, then what does?
“TLR‑4−/− mice are more susceptible to SARS-CoV than wild type mice, but experience only mild disease with no mortality in response to infection.” ―Totura, 2014
It could be worth noting that vitamin D3 has also been shown to downregulate toll‑like receptors‑2 and ‑4, two cell membrane receptors that signal through NF‑κB.
It is TLR‑2 that the spike protein of SARS has been shown to activate, an observation that perhaps best explains its increased pathogenicity relative to the innocuous coronaviruses 229E and OC43.
Toll‑like receptor‑2 is similar to TLR‑4 in a few ways, not the least being that its activation can only make things worse during viral infections.
Toll‑like receptor‑3 and RIG‑1 only two receptors expected to induce an appropriate viral response as they’re intracellular and respond to virus‑specific double‑stranded RNA.
So this immunomodulatory effect of vitamin D3 is another thing that makes it especially helpful during respiratory viral infections.
So cathelicidin is likely the reason why vitamin D3 supplementation reduces the incidence of respiratory infections in the first place…
And the downregulation of NF‑κB and TLR‑2/4 is the reason it also decreases the length of hospitalization after infection has occurred.
And even should you not be not be particularly worried about respiratory infections of any kind, vitamin D3 is essential anyway due it role in calcium homeostasis.
—-Important Message for Men Who Want to Avoid Sickness—-
This is how I’m using this simple OTC treatment to never get sick anymore
I have my own protocol for viruses, flus, and pesky sinus infections.
And since I’ve been doing this simple protocol, I have not gotten sick. My wife Jodi uses it, and she was only sick a few days over the past 18 months and it was only a slight cold.
I’ve shared this with a number of friends and students and they have not gotten sick either, or if they did it was like Jodis — gone in a few days and mild anyway.
———-

[1] Wang, Tian-Tian. "Cutting edge: 1, 25-dihydroxyvitamin D3 is a direct inducer of antimicrobial peptide gene expression." The Journal of Immunology (2004) https://www.jimmunol.org/content/jimmunol/173/5/2909.full.pdf
[2] Barlow, Peter. "Antiviral activity and increased host defense against influenza infection elicited by the human cathelicidin LL-37." PloS one (2011) https://www.napier.ac.uk/~/media/worktribe/output-200353/antiviral-activity-and-increased-host-defense-against-influenza-infection-elicited-by-the.pdf
[3] Hansdottir, Sif. "Vitamin D decreases respiratory syncytial virus induction of NF-κB–linked chemokines and cytokines in airway epithelium while maintaining the antiviral state." The journal of immunology (2010) https://www.jimmunol.org/content/jimmunol/184/2/965.full.pdf
