
[cmamad id=”18252″ align=”center” tabid=”display-desktop” mobid=”display-desktop” stg=””]
As long as your levels of this vitamin are high enough, maybe you won’t have prostate problems…
—-Important Message—–
Increase sensitivity in your penis – using this simple secret
So MUCH of today’s erection problems in men is due to desensitization. It’s a loss of feeling in the penis that comes with age, rough sex, or medications a man is taking.
And desensitization makes men unable to get or sustain hard-ons:
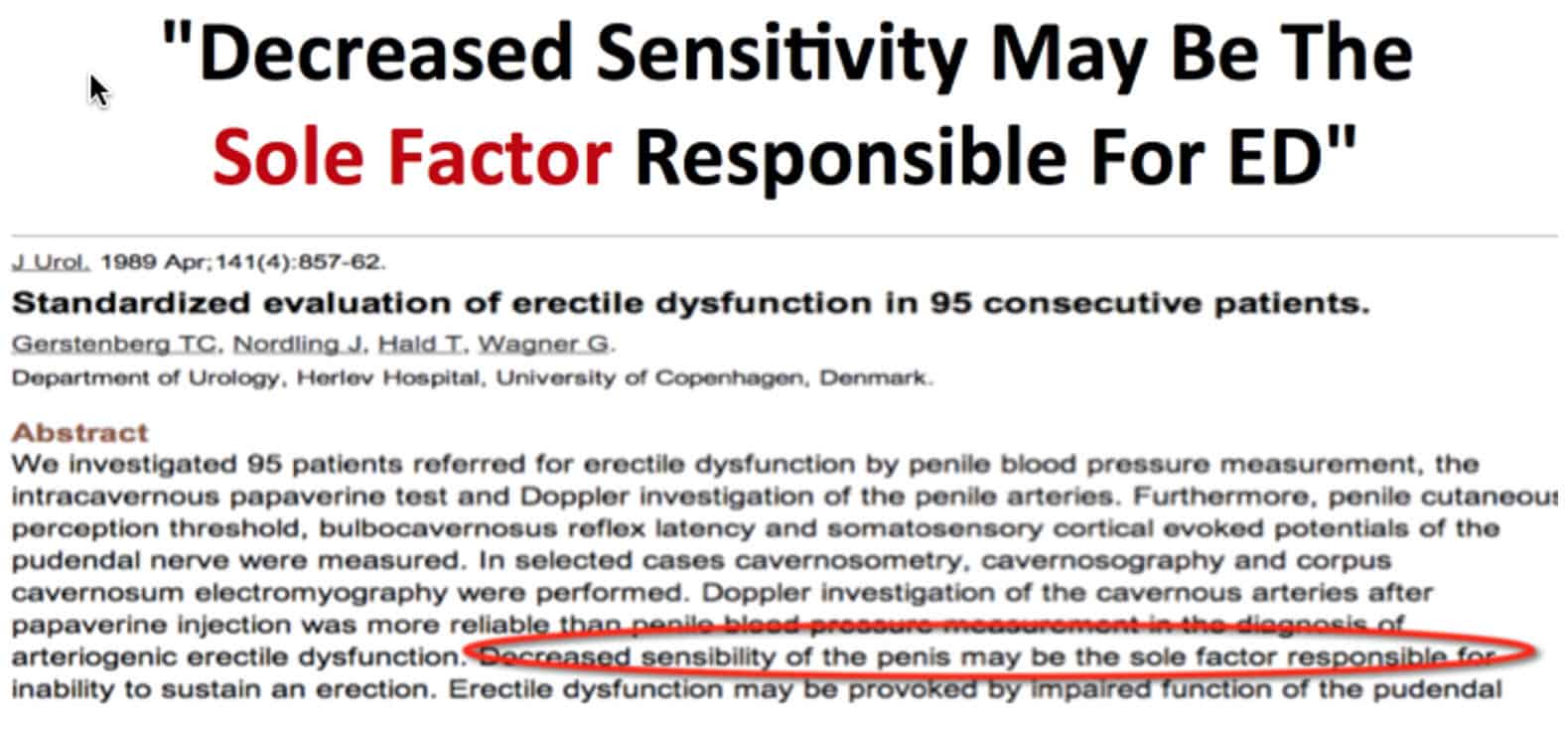
Men often have only 20% of the feeling in their penis that they should have – resulting in problems like:
- “too fast” problems
- “going soft in the middle” problems
- “can’t get an erection to begin with” problems
- “can’t feel much” problems…
…and all of these problems are often caused by desensitization.
But I found a technique that you can do by yourself, alone… and it returns all that sensitivity BACK to your penis…
I found some solo activities that help to make a man’s penis exquisitely sensitive.
Once a man does these solo activities for a few weeks, he will begin getting spontaneous woodies again, and he’ll have an erection just from a wisp of wind, ready for action… And he’ll stay hard during oh-so-pleasurable long-lasting sex…
Here’s what you need to do to replenish your sensitivity, which has been ravaged by desensitization.
——-
Most men with prostate problems are low on this vitamin
Vitamin D is associated with reduced prostate cancer risk.
Many animal studies have shown that Vitamin D is protective.
And human trials have also demonstrated this.
But even better than epidemiological studies – often confounded by measurements taken during different seasons – are the biochemical studies.
Those are very consistent.
Vitamin D always shifts the cell away from proliferation and towards differentiation…
Vitamin D is like the driver of a noisy school bus full of children – with Vitamin D at the wheel, the kids (the cells) become more focused, more disciplined, and less wild.
[cmamad id=”16490″ align=”center” tabid=”display-desktop” mobid=”display-desktop” stg=””]
With vitamin D:
- You reduce prostaglandin‐producing genes
- You increase prostaglandin‐degrading genes
- And you downregulate interleukin‐6 – a powerful cytokine that is notoriously high in prostate cancer patients
Vitamin D increases calcium, transcribes bone proteins, and lowers IGF‐1
(IGF-1 is insulin-like growth factor 1)
Its ability to reduce the cancer‐promoting prostaglandin E₂ hasn’t gone entirely unnoticed.
This effect is so powerful that some researchers have even likened vitamin D to COX‐2 inhibitors:
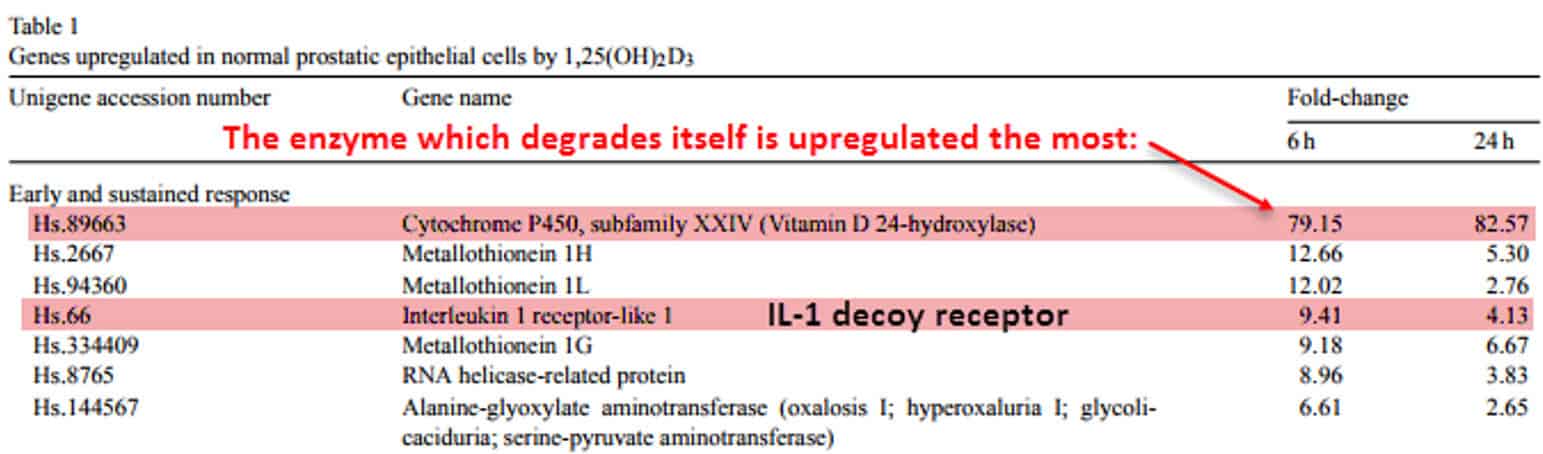
Researchers from Stanford noticed the antiproliferative effects that vitamin D had on prostate cancer cells.
So they decided to analyze these effects in more detail.
Specifically, the scientists investigated the mRNA that these cells produce.
This shows which genes are upregulated, which ones are silenced, and which ones don’t change at all.
“Our microarray data indicated that calcitriol increased the expression of 15-PGDH and significantly decreased the expression of COX-2 in LNCaP human PCa cells.”
They noticed an increase in the enzyme that degrades prostaglandins.
And that is called 15-hydroxyprostaglandin dehydrogenase.
Vitamin D also decreased cyclooxygenase‐2 – just like aspirin, indomethacin, and ibuprofen.
The ability of COX‐2 to reduce cancer risk is so well‐known that researchers have to correct for this before analyzing data…
This is similar to how smoking and drinking coffee is corrected for when analyzing Parkinson’s disease risk factors.
“Inhibition of COX‐2 by NSAIDs appeared to play a beneficial role in cancer chemoprevention.”
Anything that decreases the enzymes cyclooxygenase‐2 or ornithine decarboxylase should inhibit cancer because their products – prostaglandins and polyamines – promote growth.
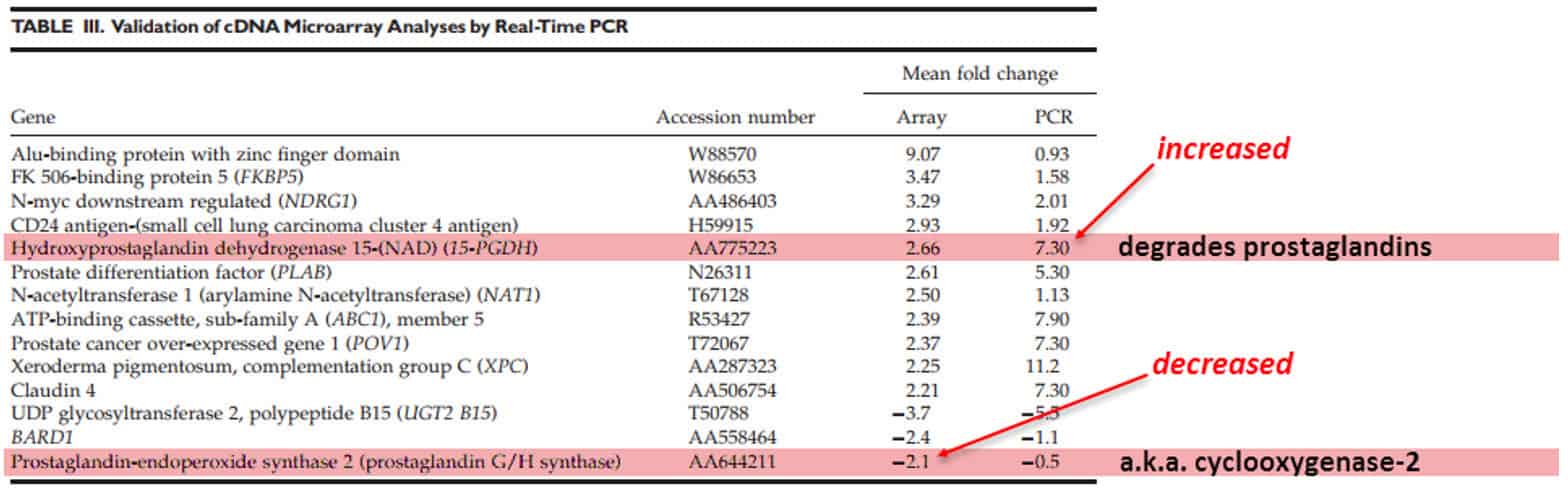
That is almost better than NSAIDs, since it also increases an enzyme which degrades prostaglandins.
Increasing this and decreasing COX‐2 would, of course, be expected to lower prostaglandin E₂.
It does as expected. This had actually been confirmed:
“This dual action was associated with decreased PGE₂ secretion into the conditioned media of PCa cells exposed to calcitriol.”
Also upregulated was the interleukin‐1 receptor‐like protein, a dummy receptor for interleukin‐1.
This binds IL‐1 while doing absolutely nothing, preventing it from causing inflammation.
It also reduced IGF‐1 by 2.22× its initial value.
Insulin-like growth factor is yet another cancer‐promoting protein that is down‐regulated by vitamin D.
It had even down‐regulated the receptors for prostaglandin E₂.
I would call this a triple‐edged sword (if there were such a thing).
“…calcitriol exerts multiple actions on the PG pathway: the suppression of PG synthesis, increase of PG catabolism, and the inhibition of PG actions (due to PG receptor down-regulation).”
Predictably, this translated to reduced growth.
With lowered prostaglandin E₂ and IGF‐1, how could it not?
And ibuprofen further increased this effect:
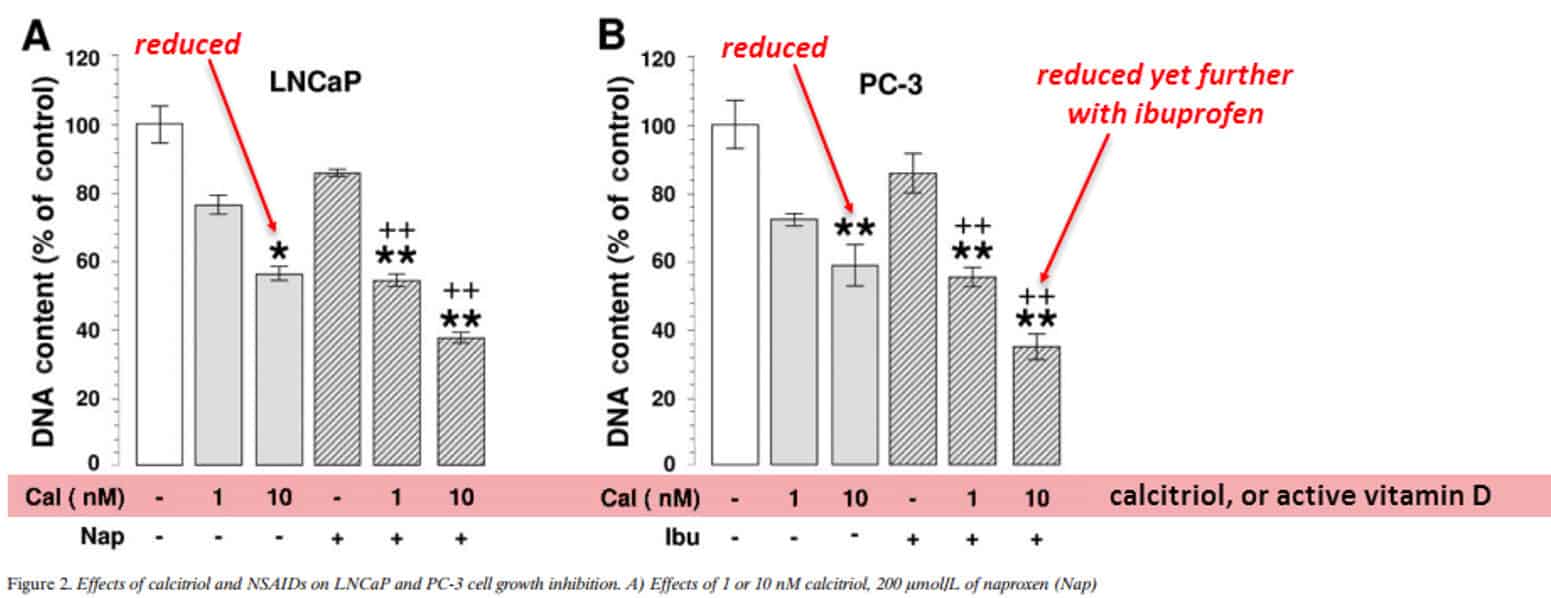
This exemplifies the powerful effect prostaglandin E₂ has in cancer.
This prostaglandin later goes on to induce ornithine decarboxylase, increase polyamines, and then rapid growth.
But there’s a slightly different type of cancer, the androgen‐resistant type.
And this is characterized by interleukin‐6:
Dipak Giri is a clinical investigator who analyzed his prostate cancer patients for interleukin‐6.
He found (as in dozens of other studies) increased interleukin‐6 levels.
This is a very consistent finding and no other cytokine is correlated like this.
“We have found that IL-6 protein concentrations are increased 18-fold in clinically localized prostate cancers when compared to normal prostate tissue and that IL-6 is secreted by normal and neoplastic prostatic epithelial cells.”
Researchers have even found that interleukin‐6 correlates better than PSA – the prostate-specific antigen.
So this cytokine attracts a good deal of research.
Prostate cancer is uniquely characterized by interleukin‐6.
“In addition, the concentration of IL-6 receptor is increased eightfold in the prostate cancer tissues.”
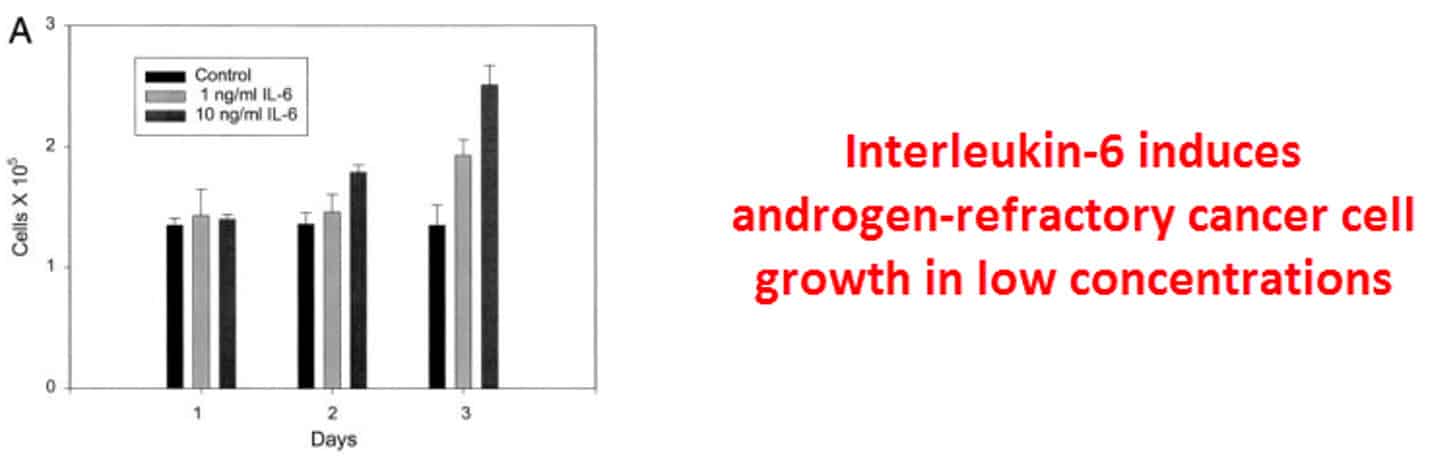
Not only is it the prostate cancer cytokine – it has been shown to increase the growth of prostate cancer cells.
And it does so at concentrations found in the body during cancer:
Not so surprisingly, interleukin‐6 acts on the cell to increase prostaglandin E₂ by inducing phospholipase A₂.
This enzyme is necessary to cleave arachidonic acid – the prostaglandin precursor molecule – from the cell membrane:
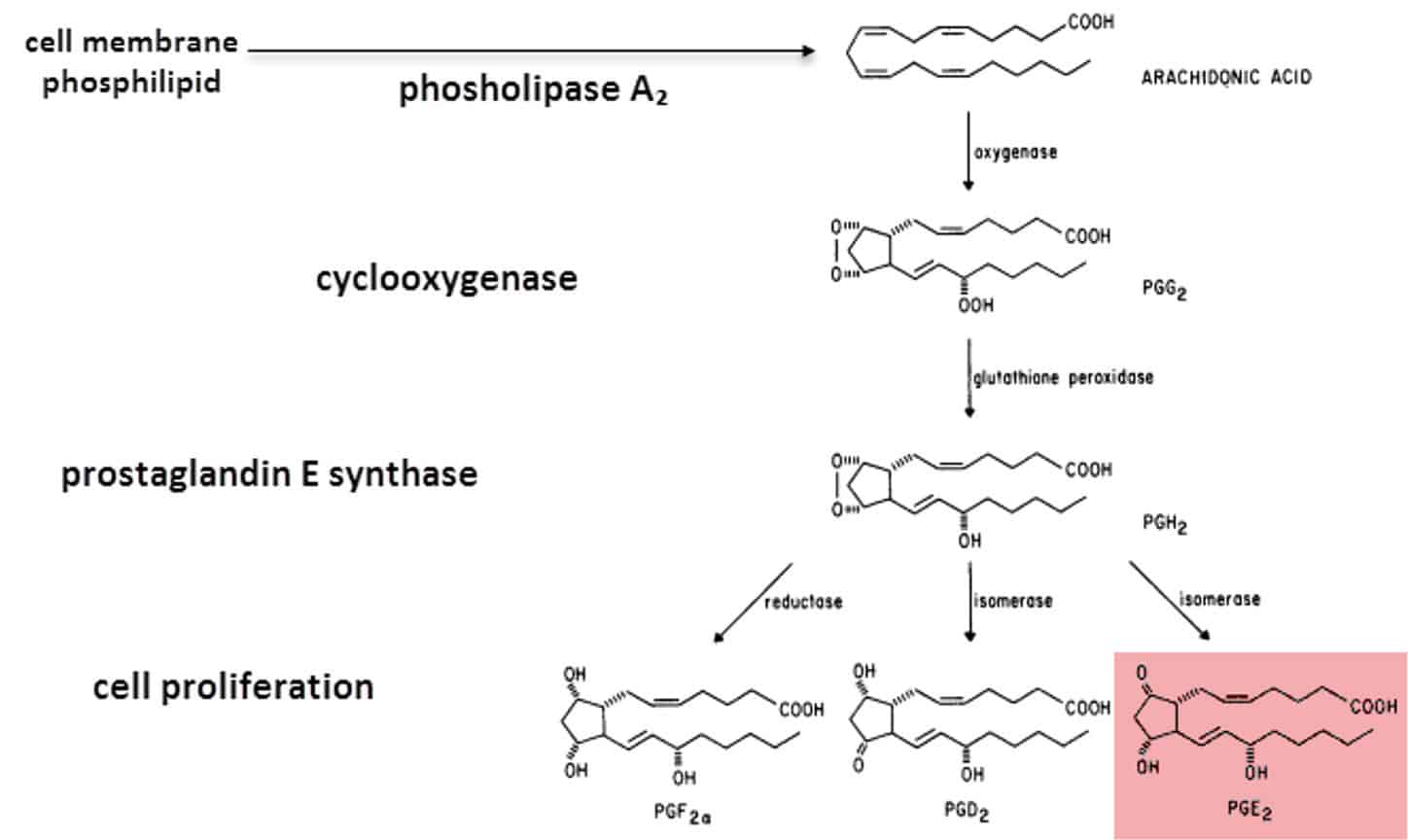
This is an especially malicious cytokine.
It creates the other enzyme (other than COX‐2) that is required to create prostaglandin E₂.
But surprisingly, vitamin D has been shown to inhibit this. Vitamin D lowers interleukin‐6.
This has been proven at least twice, and once in prostate cells:
Larisa Nonn had studied the ability of vitamin D to inhibit interleukin‐6 release in response to ultraviolet light and TNFα (tumor necrosis factor alpha).
Before this point, it had been shown to do just that in skin cells – where it caused a 75–90% reduction.
Similar reductions were noted in prostate cells.
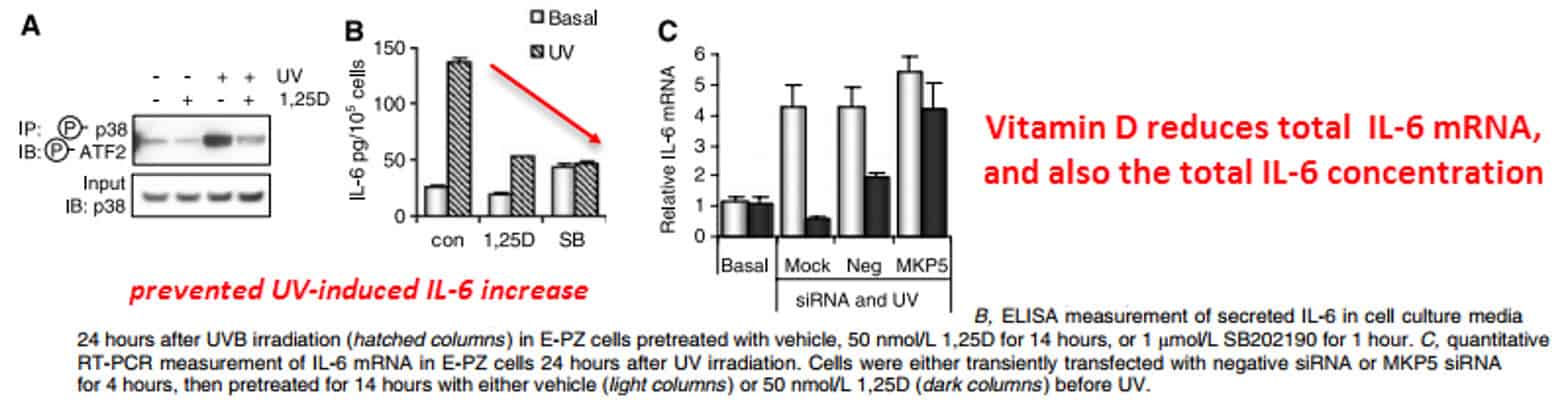
Vitamin D had also prevented TNFα (tumor necrosis factor alpha) from inducing interleukin‐6, preventing a cascade.
Cytokines can amplify each other.
“1,25D pretreatment attenuated the initial production of IL-6 and completely inhibited the accumulation of IL-6 in the media.”
Correlations between circulating vitamin D levels and prostate cancer were noted as far back as 1993.
This invited speculation on how sun exposure and latitude may affect cancer rates.
While there appears to be some truth to this, the correlations have always been confounded by things such as:
- Extremely low 200·IU doses (including measurements taken across seasons)
- Different measurement techniques and units
And blood levels never fluctuate much…
The enzyme that degrades active vitamin D is induced by itself as a negative feedback mechanism which prevents very high levels.
When all is said and done, there isn’t much but a modest fourteen-point reduction.
To get a more realistic picture, prospective studies must be examined.
This study subtype takes two groups beforehand, measures something, and then waits…
This way, it’s easier to tell what’s going on:
These researchers tracked 14,916 people over eighteen years and found 1,066 cases of prostate cancer.
Prostate cancer really is that common (NIH, 2014).
They found a risk ratio of 2.06 for aggressive prostate cancer.
This is pretty high for a study like this, with nearly fifteen thousand people:
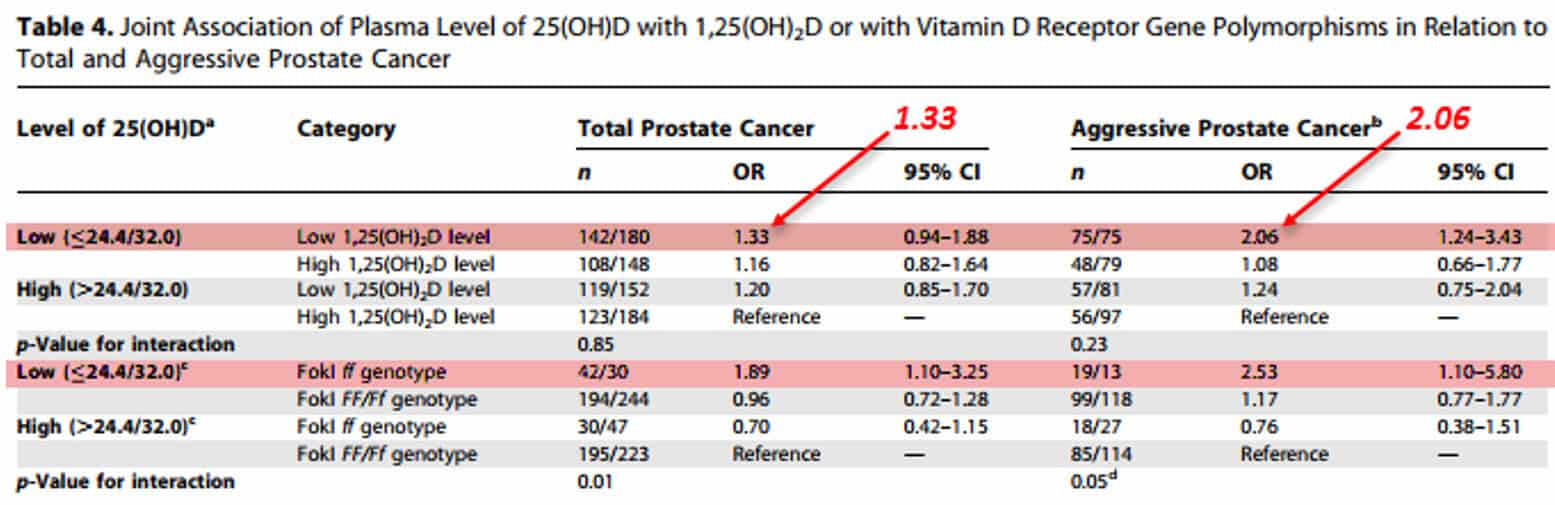
And they found genetic associations with a low‐binding vitamin D receptor variant.
This showed in another way how vitamin D levels can influence prostate cancer.
They even corrected for seasonal fluctuations.
“Compared with men whose levels of both metabolites were above the median, men with circulating 25(OH)D and 1,25(OH)₂D below the median had significantly increased risk of aggressive prostate cancer (OR 2.06).”
Scientists found the same trend in a smaller prospective study of shorter duration.
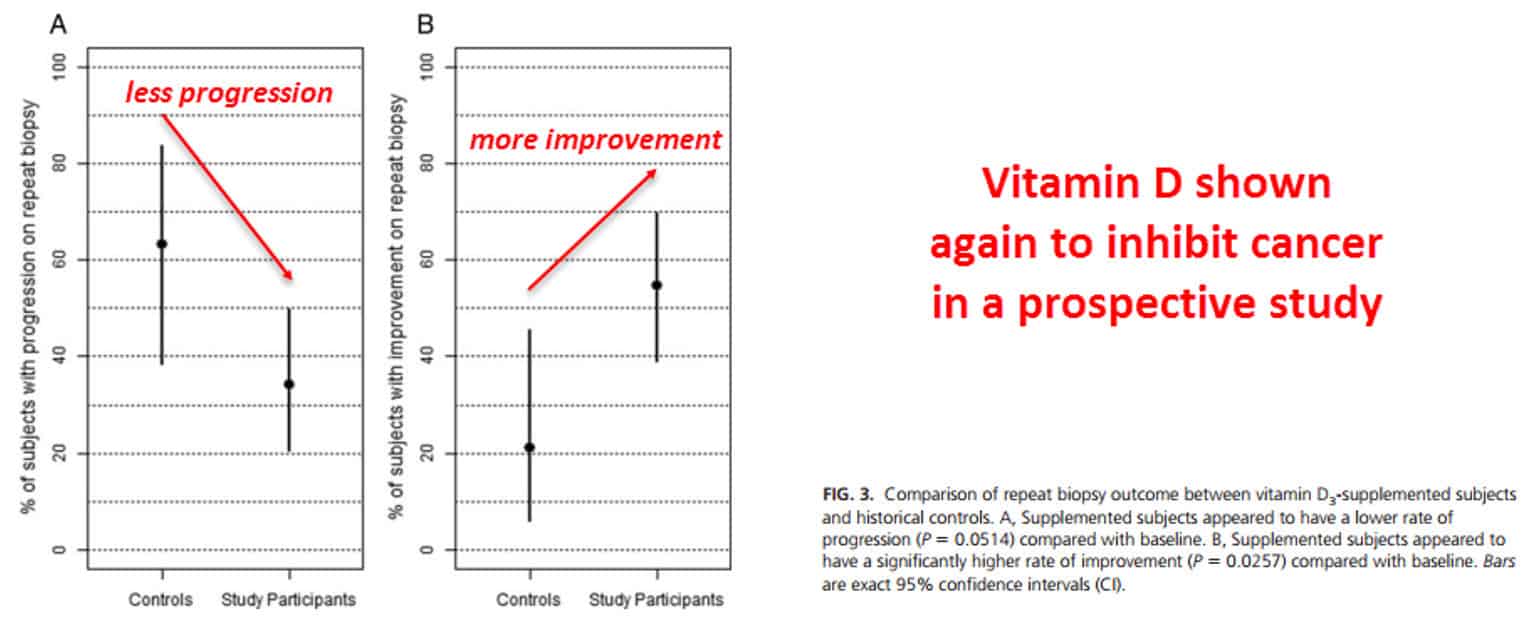
In this Marshall study, 48 subjects took 4,000·IU of Vit D per day for one year. The control subjects took none:
Studies like this are the best way to tell if it works.
Enzymes in the body keep vitamin D in range, preventing it from going over 90·ng/mL at the very most.
And the blood levels say more about recent sunlight than prior exposure.
They say little about the vitamin D stored in tissues.
“Supplementation with vitamin D₃ at 4000 IU/d for 1 yr appeared to correct all cases of vitamin D deficiency or insufficiency [..] No adverse events linked to vitamin D₃ supplementation at 4000 IU/d were observed.”
In a study analyzing vitamin D vs kidney cancer, there was a risk ratio of .31 – a threefold reduction…
And this was in the organ most exposed to vitamin D.
So Vit D is preventative – it has to be.
Vitamin D inhibits both cyclooxygenase and interleukin‐6, two enzymes that have been consistently associated with prostate cancer.
And moreover, it upregulates an enzyme that degrades prostaglandins…
It even downregulates their receptors!
“In this large prospective cohort of middle-aged US male physicians, almost one-third of the men had vitamin D deficiency (20 ng/ml), and more than two-thirds had insufficient vitamin D status (32 ng/ml) in the winter/spring.”
Although you might not expect vitamin D to diffuse and strongly inhibit cancer everywhere – to each and every location of the body – it does help!
(It does have to compete with the other steroids, after all.)
But, again, it certainly seems to help.
Vitamin D also has beneficial calcium‐absorbing functions that increase bone density.
It also transcribes for bone growth factors (i.e. BMP‐6, PLAB).
—-Important Message—-
If you are using herbs instead of vitamins – read this very important message…
Many men use certain herbs to promote their manliness, testosterone, and sexual performance…
But herbs are not designed to be used on an ongoing basis in the male body.
For example:
- Tribulus terrestris. Most products made with this plant are focused on boosting testosterone. But researchers found that Tribulus terrestris did not actually increase testosterone
- Ashwagandha. Researchers from a world-class university say that ashwagandha root extract might cause erectile dysfunction and decrease male sexual performance.
- Yohimbe was given to patients with ED problems, but 65% had no positive result at all, according to a Brown University study.
- Ginseng. A study done years ago showed that ginseng does not seem to increase testosterone. Common side effects include headache, agitation, upset stomach, and dizziness. An increase or decrease in blood pressure may also occur.
- Siberian ginseng may also cause drowsiness, nervousness, or mood changes.
As you can see, vitamins are a much safer choice than herbs. But what vitamins should a man take for better sexual performance and stamina?
Here’s the amazing vitamin alternative to dangerous and ineffective herbs
————-


Leave a Reply