
Urgent bulletin for people who love chicken…including the safe way to eat chicken…
—-Important Message for Men in Pain—-
This “manly element” naturally relieves arthritis and joint pain by 71%
Dr. Rex Newnham developed arthritis while working as a plant and soil scientist in Australia in the 60s…
And he found no relief with traditional treatments — which is why he turned to plants and natural remedies.
And after years of experimentation, he identified this one Manly Element as a powerful, natural arthritis cure.
And it’s so cheap, and so readily available…plus you only need a tiny teaspoon amount…
Here’s what one man says about using the Manly Element for his pain:
Here’s how to get this cheap natural arthritis cure — relieves pain by 71%
———-
How nibbling chicken bones causes severe arthritis
Chicken bones may be responsible for terrible arthritis and joint pain.
In today’s newsletter, to show you how, we are going to first visit the idea that an infectious agent…
…specifically yeast/fungi, as being responsible for many cases of arthritis.
Then we’re going to show you how chicken bones are a chief culprit.
Let’s begin…
Why is it that antifungals are effective in treating about half of all cases of arthritis?
Borates are general antifungals that work by crosslinking cellulose and chitin, the latter being a necessary cell wall component of yeast and fungi.
This would imply that there is another unknown cause underlying the condition.
The “Herxheimer reactions” that directly precede arthritis remissions, as described by Newnham and others (Wyburn-Mason, 1983), are testament to its often infectious nature.
“The occurrence of the Herxheimer reaction in rheumatoid diseases, including its extra-articular and autoimmune lesions, with the above drugs is highly significant.” (Wyburn-Mason, 1983)
And there is also the occurrence of YKL-40 in about 60% of all rheumatic cases (Johansen, 1999).
YKL-40 is a circulating chitin-binding protein created by the immune system – ostensibly to kill yeast/fungi.
The similarity of YKL-40 to mammalian chitinase, a chitin-hydrolyzing enzyme, implies a function in antifungal immunity.
Bacteria do not produce chitin, and mammals don’t either.
Because only yeast, fungi, insects, and shellfish produce chitin, we can suppose the presence of YKL-40 is a biomarker for yeast/fungi.
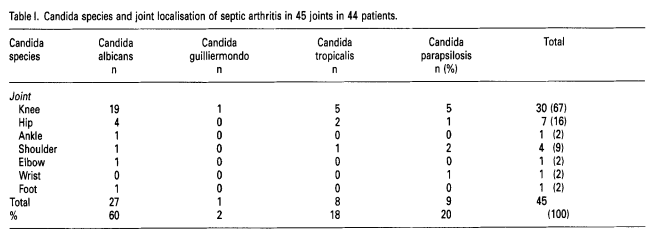
The existence of fungal arthritis is in no way speculative.
But there could be disputes about its general prevalence.
There are review articles on fungal arthritis (Cuellar, 1992). And dozens of different species have been isolated from arthritic joints (Hansen, 1995).
Yet there is another way to induce arthritis that is completely independent of microbes of any type.
It was shown as far back as the mid-1970s that injections of Type II collagen will reliably lead to arthritis in approximately half of all rats (Trentham, 1977).
|
The most common types of collagen (from Wikipedia): Type I: skin, tendon, vasculature, organs, bone Type II: cartilage (and Type XI is another cartilage type) Type III: reticulate (in supporting mesh of bone marrow and other soft tissues), commonly found alongside Type I Type IV: forms basal lamina (in things such as blood vessels and gastrointestinal tract) Type V: cell surfaces, hair, and placenta |
“…Types II and XI are the only collagens that have been shown to be arthritogenic; collagen types I and III do not induce autoimmune reactions.”
Furthermore, the transfer of anti-collagen antibodies from arthritic rats to normal rats induces arthritis in the normal rats (Wooley, 1984).
This dispels any doubt surrounding the causative nature of anti-collagen antibodies, proving that these act to mark the joints for destruction.
Shortly thereafter, the effect was confirmed in nonhuman primates (Yoo, 1988).
And this renewed scientific interest in the collagen Type II auto-antibodies found in patients with rheumatoid arthritis.
“It is noteworthy that the rheumatoid cartilage extracts contained 14 and 37 times more IgG and IgM, respectively, than did the normal cartilage extracts…” (Jasin)
Such demonstrations of collagen-induced arthritis led to dozens of publications.
And these, taken as a whole, strongly suggest that about 60% of all rheumatic cases are autoimmune in nature.
Here are a few articles that exemplify just how autoimmune arthritis could occur, why this is expected, and exactly which common dietary item is likely causing it:
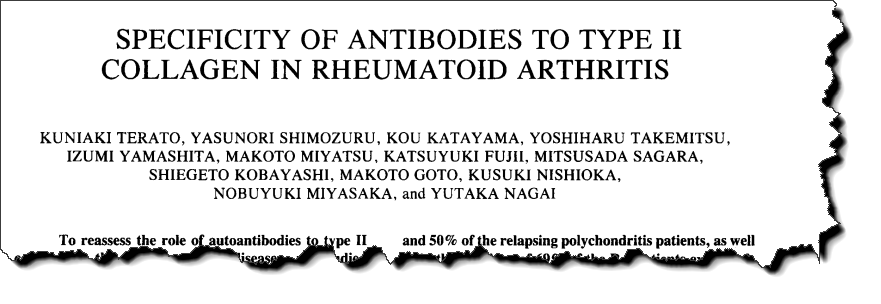
Of the scores of articles on this topic, this one is perhaps the most comprehensive.
The author tested both serum and cartilage for auto-antibodies, and speaks plainly about their likely origin and some unpublished observations.
“These results indicate that the auto-antibodies in rheumatoid arthritis sera bind specifically to the cartilage.”
They didn’t test the synovial fluid (a fluid in joints) specifically.
But previous studies unanimously reveal that it would be expected to contain auto-antibodies in concentrations intermediate between plasma and cartilage.
But most importantly, Dr. Kuniaki Turato tested the cross-reactivity of the antibodies towards collagen Type II in monkey, rat, bovine (i.e. cows), mouse, and chicken.
This is crucial – because if these had a dietary origin it could help us know which animal species to avoid eating.
Of course, ingesting skin collagens would never be an issue regardless of species – these contain collagen Type I and Type III.
But some cuts of meat that people eat contain collagen Type II.
“Hence, it is of utmost importance to test the present hypothesis that denatured Type II collagens in the diet play a role in the stimulation of auto-antibody formation.”
Collagen Type II is, more or less, exclusively a cartilage protein.
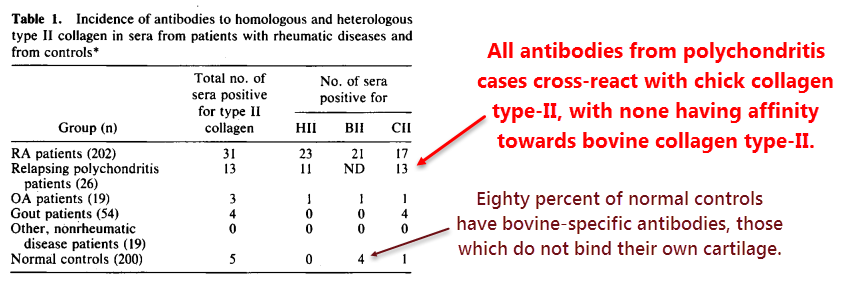
Terato’s data strongly suggests that, when considering humans, chicken collagen is more cross-reactive than bovine collagen:
Relapsing polychondritis (see graphic above) involves everything rheumatoid arthritis does and then some, as this condition also affects collagen Type II of the nose and ears.
Polychondritis can even cause deformity after a few relapses.
And death can occur should bronchial or laryngeal cartilage be involved.
All the gout and polychondritis patients had only chicken-reactive antibodies in their serum…
…while most of the controls (80%) had bovine-reactive antibodies, which are apparently innocuous.
It would logically follow that chicken collagen Type II is more cross-reactive with our own collagen Type II, and thus far most likely to be the true causative agent.
“Furthermore, severe arthritis can be induced in…monkeys by immunization with chick CB-11, CB-10, and CB-12… The anti-Type II collagen antibodies produced by both of these species [chicken and bovine] definitely cross-react with native homologous Type II collagen.”
Even though the rheumatoid arthritis patients had an approximately equal number of antibodies that cross-react with each species (either bovine or chicken) this data does not prove which is responsible.
When adding together the chicken and bovine columns (in the table) you get 38, a value nearly twice that of 23 – the number of total autoimmune cases.
This could imply that one of the two antibody types, either chicken-reactive or bovine-reactive, is merely an innocent bystander.
“These findings suggest that some anti-collagen antibodies might have been stimulated by denatured collagen and degraded collagen products that were absorbed from the gastrointestinal tract.”
It would seem logical that some rheumatoid arthritis cases have a deficiency in pancreatic and/or salivary collagenase (Uitto, 1990).
Collagenase is an enzyme capable of degrading the tightly-wound triple helix of collagen, something most stomach enzymes cannot accomplish.
A collagenase deficiency could explain the presence of both antibody specificities…
Yet only one needs to be pathogenic for arthritis to occur.
The fact that most of the auto-antibodies were of the IgA class (those formed upon dietary ingestion) also implies that a dietary role often underlies rheumatoid arthritis.
‘The incidence of IgA anti-Type II collagen antibody-positive sera was found to be twice as high as that of IgG antibody-positive sera…”
The comparison of the polychondritis group versus the controls strongly implicates chicken and not bovine collagen…
And you don’t have to go far for supporting evidence:
For an antibody to be created against an ingested protein, it must first get into the body as a fragment that is more than ~12 amino acids in length.
Anything shorter than this and you are fine…
And that’s the reason why proper digestion and enzyme supplements are protection against certain autoimmune diseases.
But the protein also needs to be similar enough to our own to elicit auto-antibodies, yet still different enough for the immune response to occur in the first place.
So even though we all probably have antibodies against something we are eating at the moment…
…chances are they don’t bind to anything important besides the food they’d been created against.
And we also ingest some proteins so similar to our own that no response of any kind actually occurs from this.
So antibody cross-reactivity is of paramount importance and is highly species-specific.
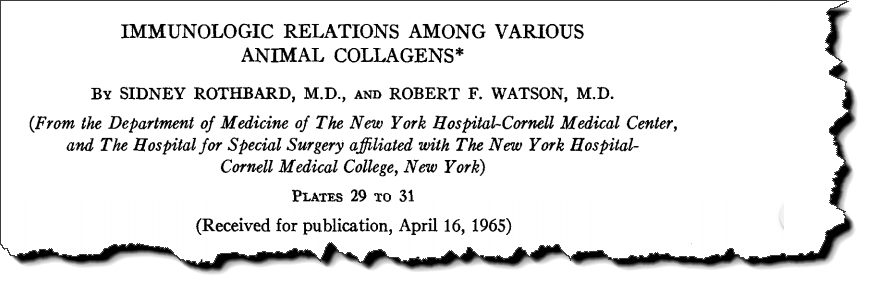
This is why Professor Sidney Rothbard tested cross-reactivities of collagens derived from six species: rat, mouse, guinea pig, human, chicken, and carp.
He determined cross-reactivity in two ways:
(1) He took antibodies specific towards the collagens of each species and injected them into each and every species (with the exception of human) in a round-robin manner.
(2) He did direct binding studies using collagens of every species along with their antibodies.
The cross-reactivity between human and chicken collagen was remarkable:
“Human and chicken collagen showed marked reciprocal cross-reactions.”
Although the proteins he used were extracted from skin, and were thus collagens Type I and Type III, the results are still suggestive…
“The collagens Type I and Type III derived from cows and pigs…were so unreactive as to be used as implant material…” (Lynn, 2004).
One study found that, of 345,000 collagen implant recipients, only eight had immunological reactions (Cukier, 1993).
Chicken collagen is never used for implants, and it seems there is good reason for that.

And there is more evidence:
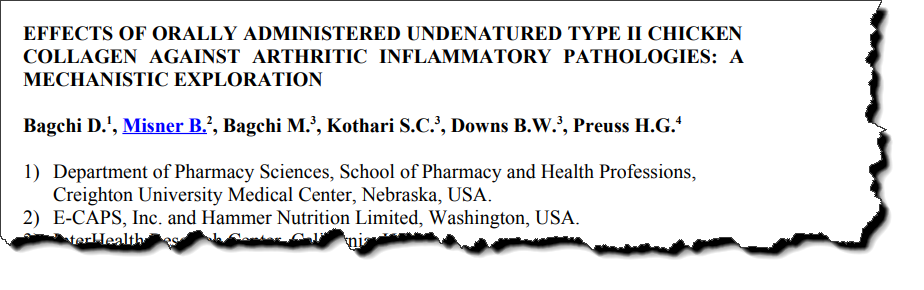
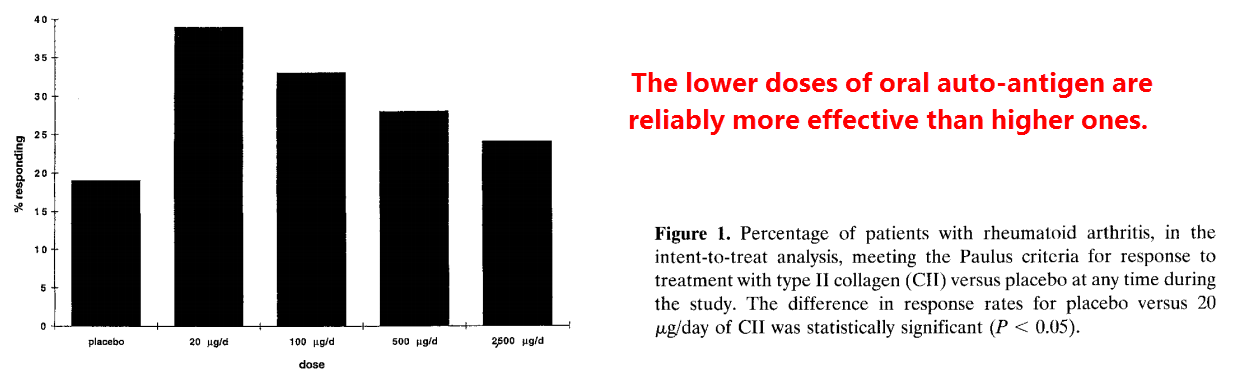
In this study, they gave low oral doses of chicken collagen Type II to patients with rheumatoid arthritis.
The administration of auto-antigens is often done with autoimmune diseases to promote tolerance and reduce symptoms.
Rheumatoid arthritis is no exception, and many studies verify that this really works.
The fact that this really does work implies that chicken collagen is the true auto-antigen.
This would mean, although not explicitly stated, that the consumption of chicken cartilage had actually caused the condition.
“Oral administration of auto-antigens has been shown to suppress a variety of experimentally induced autoimmune pathologies, including antigen-induced rheumatoid arthritis.”
This “tolerance” is often explained through gut-associated lymphoid tissue (GALT), yet I find those explanations to fall short of the mark.
Mechanistic explanations underlying auto-antigen “tolerance” basically just come down to mentioning which particular cytokines are induced, as if that alone must somehow do it (Weiner, 1997).
Yet the very same articles present proof that this works regardless of the route of delivery – either injected or ingested.
This form of “tolerance” has even been shown to work via intranasal administration (Daniel, 1996), proving this has nothing to do with gut-associated lymphoid tissue.
So, basically, the mainstream explanation really explains nothing and often contradicts itself.
It is much more likely, in my view, that the ingested collagen is actually binding (and thus neutralizing) the auto-antibodies circulating in the bloodstream.
This would explain why a lower dose works better (Barnett, 1998)…
Too much auto-antigen would equate to eliciting more auto-antibodies.
Oral tolerance doesn’t work with denatured collagen, implying that gelatin should be safe even it it were actually cross-reactive:
The collagen must be in triple-helical form. And this is because the antibodies that are created against single strands do not bind triple-helical collagen as strongly.
“In rheumatoid arthritis, a 280-patient, double-blind Phase II dosing trial of chicken Type II collagen in doses ranging 20-2500 μg demonstrated statistically significant positive effects in the group treated with the lowest dose…” (M.L. Barnett)”
“Oral administration of larger doses of bovine Type II collagen (1-10 mg) did not show a significant difference between tested and placebo groups, although a higher prevalence of responders was reported for the groups treated with Type II collagen.” (Weiner)
Going further along this line, you’d expect collagen that’s been cooked in water to be safer.
This is because hot water is effective at swelling and then unwinding the coil.
Besides chicken being high on the suspect list based on interspecies cross-reactivity, this bird is also a relatively dry meat – especially when fried in anhydrous oil.
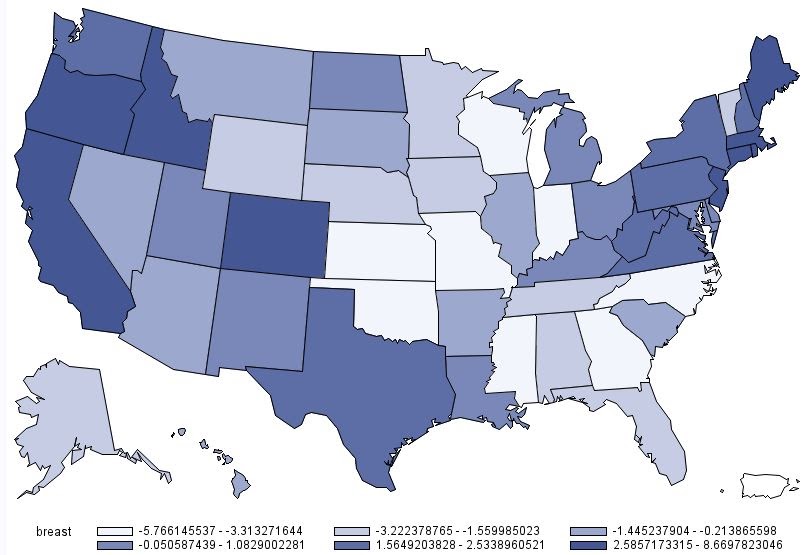
This could be the reason why the US map of rheumatoid arthritis (below) resembles that of chicken wing demand (below that one) more closely than that for chicken breast demand (further below).
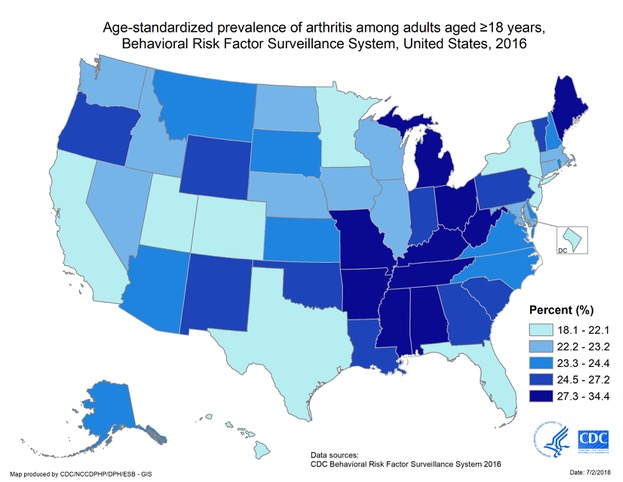
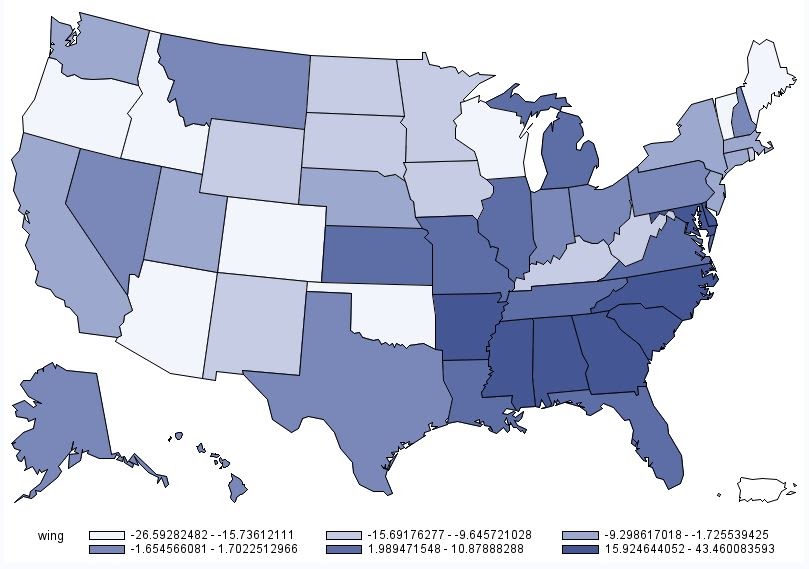
The other reason, of course, is that chicken breast has less cartilage and hence less collagen Type II than do wings and legs.
But you could still expect chicken legs could be safe when thoroughly cooked in water, as under those conditions the collagen triple helix may unfurl.
Besides providing more indirect evidence that chicken collagen Type II is the auto-antigen of rheumatoid arthritis, Dr. Bagchi had also shown that approximately half of triple-helical collagen survives digestion.
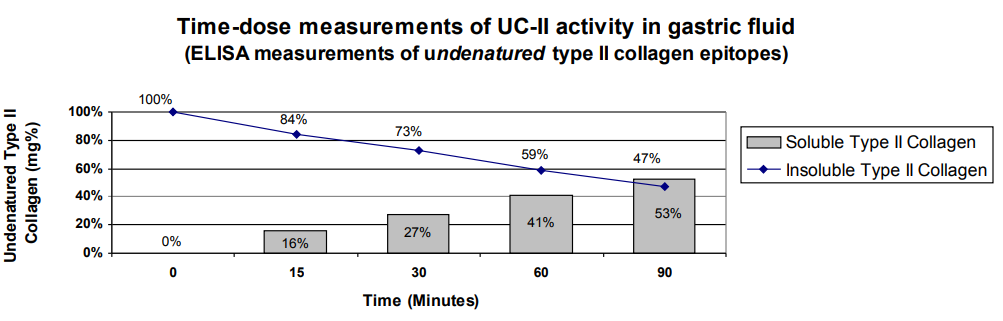
He used pepsin at pH 2.0 for 1.5 hours but hadn’t supplied collagenase.
That enzyme can digest helical collagen even though pepsin cannot, and isoforms have been found in the saliva and pancreas (Houck, 1959).
Even though helical collagen is resistant to pepsin hydrolysis, which is actually used to isolate it from skin, gelatin is efficiently degraded by this enzyme.
This is yet another reason why consuming cow gelatin is likely to be a non-issue…
Because any long antigenic fragments that may be present would be reduced to a non-immunogenic size anyway.
Bromelain (an enzyme in pineapple) is so notorious for digesting gelatin that pineapple is contraindicated in making Jello – yet it will do nothing to helical collagen.
Believe it or not, bromelain actually speeds up healing time (Wu, 2012).
The “arthritis hotspot countries” – such as Jamaica and Mauritius – may truly have low boron levels (though Newnham doesn’t supply much evidence for this).
But they are also notorious chicken-consuming countries.
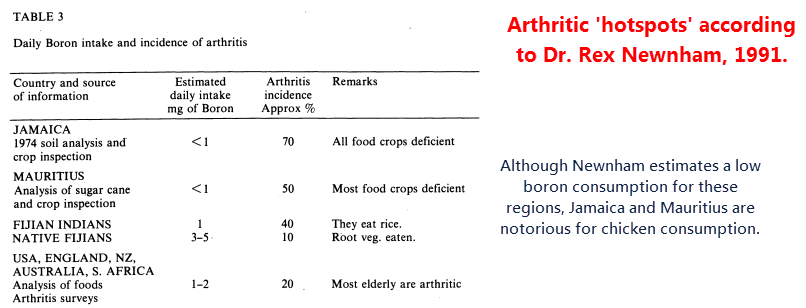
These small island nations don’t have the space for cattle…
But they don’t care because they have a considerable proclivity for fried chicken:
- Mauritius consumes 38.1 kg per person per year
- Jamaica consumes 51.3 kg per person per year
And they have lots of arthritis.
Of course, you wouldn’t exactly want to eat fried chicken anyway, which has no redeeming qualities (besides its wonderful taste and irresistible texture) and is high in bad PUFA fats.
Chickens are often fed low-priced temperate seeds, such as soy and corn, and thus acquire a terrible fatty acid profile high in linoleic acid.
“…Carp collagen, alone of those tested, showed no cross-reactions.” (Rothbard)
Yet chicken breast is so low in fat that it matters little, and seeing as it’s also low in collagen Type II it’s probably not an issue to eat boneless skinless chicken breasts (as I do when I consume chicken.)
And there is one more line of proof worth mentioning:
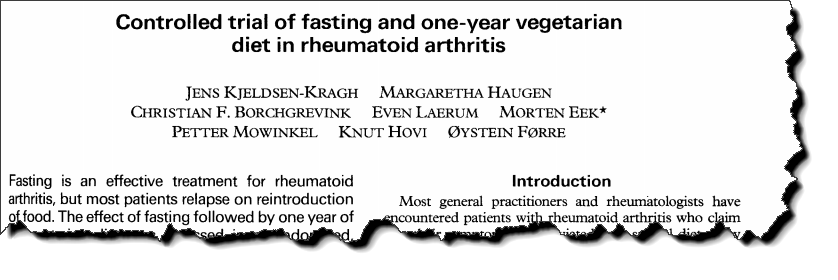
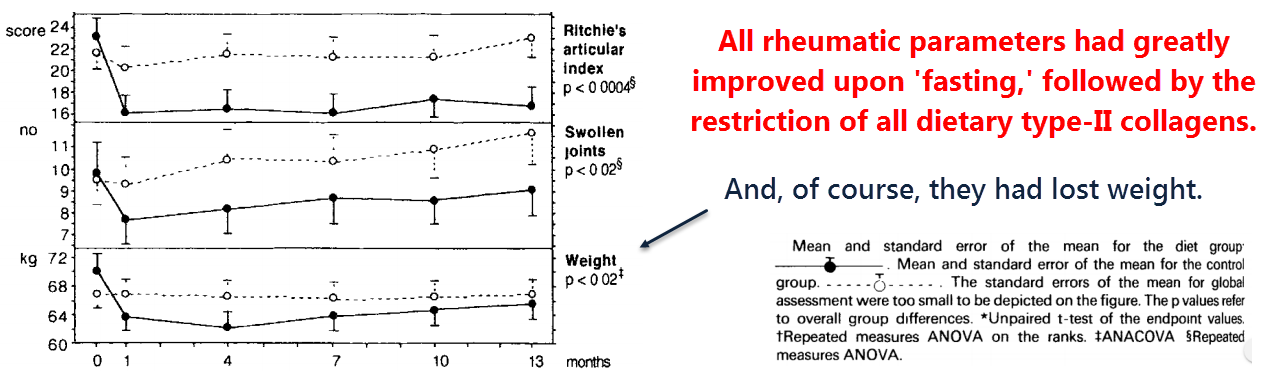
This Norwegian study showed that a 7 to 10-day semi-fast of mostly vegetable broth and juice, followed by a lacto-vegetarian diet for several months, greatly improved rheumatoid arthritis symptoms in all 27 subjects.
And in the same study, the 26 controls, eating their normal diet, deteriorated.
“Fasting is an effective treatment for rheumatoid arthritis, but most patients relapse on reintroduction of food.”
“…that an individually adjusted diet reduces disease activity suggests that food allergy or intolerance is involved to some degree in the pathogenesis of rheumatoid arthritis.”
So what does this tell us about food and rheumatoid arthritis?
The Norwegian study greatly implicates either chicken, beef, pork, or fish…
But since only chicken collagen had been proven cross-reactive, I would strongly suspect that.
Besides having a much better fatty acid profile and being less immunogenic, beef is more hydrated, probably hydrolyzing any collagen Type II during cooking.

Flash-fried chicken legs, however, are drier and are often cooked too quickly from the outside.
Moreover, fried chicken is often served in restaurants where speed is the prime concern.
“Most general practitioners and rheumatologists have encountered patients with rheumatoid arthritis who claim that their symptoms are alleviated by a special diet or by simple elimination of certain items from the usual diet. Such reports tend to be viewed with skepticism…”
It’s been shown that entire starch particles can be persorbed whole (Volkheimer, 1968), and also that the same is possible with entire proteins (Ross, 1980).
The Bagchi article above shows that triple-helical collagen is only half degraded during 90 minutes of simulated stomach conditions.
And that was without any oil to protect it.
I think it’s fair to assume that eating fried chicken could lead to helical collagen Type II becoming encapsulated within PUFA liposomes upon ingestion, perhaps leading to an autoimmune state should antibodies be formed against it.
Chicken nuggets are often made with mechanically deboned chicken, so cartilage fragments could be expected.
Here is one anecdote, taken from an article about food-induced arthritis:
“Our patient’s status may have deteriorated when she received chicken, beef, and rice… Although her clinical status changed following challenge with these foods, the chicken and beef challenges were close together, temporarily, making interpretation difficult. Circumstances have not yet permitted rechallenge with these foods to confirm these tentative observations… She may also have reacted to rice, chicken, or beef, but we have thus far not had opportunities to reproduce observations with these particular foods.” (Panush, 1986)
—-Important Message—-
This food ingredient should be outlawed — how much did you eat today?

This bad ingredient is in MOST of today’s foods…
…it builds up in the bloodstream and travels to different parts of the body…
It builds up in a man’s Leydig cells in the testicles, making his testosterone plummet…
It destroys the beta cells in the pancreas, so men become insulin resistant and get diabetes…
…and it builds up in a man’s penile chambers, blocking good blood flow and causing “rockiness” problems.
———-
